|
Algorithm for Management of Pressure Ulcers/Injuries
|
TREATMENT
Overview
This topic covers management of pressure ulcers/injuries (PUs/PIs). For clinical guidelines and quality measures specific to PU/PI, see "Pressure Ulcers/Injuries - Overview". For an introduction and assessment of PU/PI including epidemiology, risk factors, etiology, pathophysiology, history, physical examination, diagnosis, differential diagnoses, documentation and ICD-10 coding, see "Pressure Ulcers/Injuries - Introduction and Assessment". For PU/PI classification systems, with pictures and descriptions, see "Pressure Ulcers/Injuries - Classification/Staging". For prevention strategies, see "Pressure Ulcers/Injuries - Prevention". For best practices in care coordination, see "Pressure Ulcers/Injuries -Coordination of Care".
Background
Coordination of care is an important aspect for management of PUs/PIs, as patients tend to have co-morbidities usually treated by different healthcare teams across different care settings (e.g., acute care, patient's home, wound clinic etc). PUs/PIs are best managed by a multidisciplinary team, which creates a customized treatment plan based on the patient's input and based on a comprehensive assessment that:
- Identifies underlying causes of the PU/PI and assesses risk factors contributing to development of PUs/PIs, delayed healing, and infections
- Differentiates from other types of lower extremity ulcers, which require different treatments
- Identifies pertinent patient's/caregiver's concerns
- Categorizes PU/PI using a validated classification system, such as the one developed by the National Pressure Ulcer Advisory Panel (NPUAP).[1] See "Pressure Ulcers/Injuries - Classification/Staging".
-
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
- Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis or serum-filled blister
- Stage 3 Pressure Injury: Full-thickness skin loss (i.e., without exposed fascia, muscle, tendon, ligament, cartilage and/or bone)
- Stage 4 Pressure Injury: Full-thickness skin and tissue loss (i.e., with exposed fascia, muscle, tendon, ligament, cartilage and/or bone)
- Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss (i.e. extent cannot be determined due to presence of slough and/or eschar)
- Deep Tissue Pressure Injury (i.e. intact or non-intact skin with non-blanchable maroon/purple discoloration or a blood-filled blister)
- Determines ulcer prognosis or "healability", that is, the potential of the ulcer to heal with conservative treatment only.[2][3] For details, see 'Ulcer healability' in "Pressure Ulcers/Injuries - Introduction and Assessment":
-
- Healable: underlying cause of the ulcer can be treated, patient adheres to treatment and there are no factors that impede ability to heal
- Maintenance: ulcer has healing potential but patient or health system barriers compromise healing
- Non-healable: underlying cause cannot be treated conservatively, or blood supply to the wound is inadequate (e.g., critical limb ischemia), or co-factors impede ulcer healing (e.g., terminal organ failure, ulcer is a malignant tumor). If cause or co-morbidities impeding healing cannot be treated with a conservative approach but can be surgically treated, surgical consult/ referral is recommended. If patient is a poor surgical candidate, ulcer is treated as non-healable.
An adequate treatment plan for PU/PI aims to[2][3]:
- Treat the cause and other factors impeding healing
- Assess patient's and caregiver's concerns
- Provide effective local wound care
If a healable PU/PI does not show any signs of improvement within 2-4 weeks despite adequate treatment, treatment plan should be reassessed, differential diagnoses re-evaluated and adjunctive therapies considered.[1][4]
Of note, in all practice settings, it is essential to ensure that the treatment plan and care provided adheres to the specific facility's policies, procedures, protocols, and formulary.
See Algorithm for Management of Pressure Ulcers/Injuries (Algorithm 1)
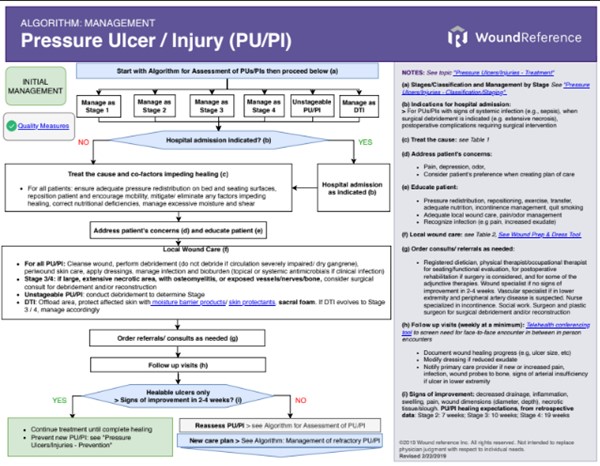
Algorithm 1. Algorithm for Management of Pressure Ulcers/Injuries (click on this link to enlarge)
Treatment goals
Healable PU/PI
- In general, goals for healable PUs/PIs are to address underlying contributing factors (e.g. by providing pressure redistribution with support surfaces and repositioning) to promote wound healing, to prevent recurrence and provide appropriate psychosocial support. Patient's concerns that may not be initially obvious need to be taken into account when creating a treatment or care plan.
- For a healable PU/PI, if the area of the ulcer does not show signs of improvement despite 2-4 weeks of adequate treatment, the ulcer, patient and plan need to be reassessed. [1][4] See 'Plan Reassessment' and 'Adjunctive Therapy'.
Non-healable or maintenance PU/PI
- For maintenance PUs/PIs, goals may include addressing patient or health system barriers that prevent an otherwise healable wound from healing. While barriers persist, ulcer is managed as a non-healable ulcer.
- For maintenance or non-healable PUs/PIs, if cause or co-morbidities impeding healing cannot be treated with a conservative approach but can be surgically treated, surgical consult is recommended. If patient is a poor surgical candidate (e.g., patient cannot tolerate anesthesia), ulcer is treated as non-healable. Palliative wound care goals include prevention of ulcer progression, and symptom control (e.g., management of pain, odor, exudate). Patient's quality of life, concerns and comfort should be prioritized when creating a treatment or care plan.[5]
Management by Ulcer Stage
Table 1 below summarizes initial management for healable PUs/PIs, based on the latest clinical guidelines by the National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (NPUAP/EPUAP/PPPI), Wound Healing Society (WHS), Wound, Ostomy and Continence Nurses (WOCN) Society, National Institute for Health and Care Excellence (NICE), and expert opinion.[6][7][8][9][10][11]
- Of note, blanchable erythema (normal reactive hyperemia) is seen when a skin area that is reddened turns pale as a result of applying pressure with a finger or plastic disc and preventing blood flow to the region. As the pressure is released, skin turns red again.[6] Blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes [1] and represent an opportunity to implement offloading and pressure redistribution strategies before further skin damage occurs.
Table 1. Management of healable PUs/PIs by ulcer stage
| Stage |
Treat the Cause |
Local Wound Care |
|
Stage 1
(Non-blanchable erythema of intact skin)
|
-
Manage underlying causes
-
Pressure redistribution: Assess need for support surface. If it is needed, start with high specification reactive foam mattress or non-powered pressure redistribution support surface (Group 1)[6] If PU/PI is in heel: float the heel
-
Reposition patient and encourage mobility, if not contraindicated
- Optimize nutrition
- Address excessive moisture and shear: manage incontinence if needed
|
- Protect affected skin with moisture barrier products and skin protectants
|
|
Stage 2
(Partial-thickness skin loss with exposed dermis or serum-filled blister)
|
-
Manage underlying causes
-
Pressure redistribution: Assess need for support surface. If it is needed, start with high specification reactive foam mattress or non-powered pressure redistribution support surface (Group 1)[6], may progress to a powered pressure reducing air mattresses or similar (Group 2) if needed. If PU/PI is in heel: float the heel
-
Reposition patient and encourage mobility, if not contraindicated
- Optimize nutrition
- Address excessive moisture and shear: manage incontinence if needed
|
Comprehensive local wound care including cleansing, control of bioburden, barrier cream or wound moisture balance with appropriate dressing and periwound skin protection
|
|
Stage 3
(Full-thickness skin loss - without exposed fascia, muscle, tendon, ligament, cartilage and/or bone)
|
-
Manage underlying causes
-
Pressure redistribution: if large or multiple stage 3 or 4 ulcers on trunk or pelvis, or if patient has recently had a flap to close PU/PI, may use group 2 support surfaces (powered air flotation beds, powered pressure reducing air mattresses, non-powered advanced pressure reducing mattresses). If PU/PI is on heel: completely offload the heel
-
Reposition patient and encourage mobility, if not contraindicated
- Optimize nutrition
- Address excessive moisture and shear: manage incontinence if needed
|
-
Comprehensive local wound care including cleansing, debridement, control of bioburden, wound moisture balance with appropriate dressings and periwound skin protection
- Consider surgical reconstruction with flaps if ulcer is large
-
Consider use of adjunctive therapy
|
|
Stage 4
(Full-thickness skin and tissue loss - with exposed fascia, muscle, tendon, ligament, cartilage and/or bone)
|
-
Manage underlying causes
-
Pressure redistribution: if large or multiple stage 3 or 4 ulcers on trunk or pelvis, or if patient has recently had a flap to close PU/PI, may use group 2 support surfaces (powered air flotation beds, powered pressure reducing air mattresses, non-powered advanced pressure reducing mattresses). If PU/PI is on heel: completely offload the heel. Sitting on wheelchair is not recommended except for emergencies or important issues.
-
Reposition patient and encourage mobility, if not contraindicated
- Optimize nutrition
- Address excessive moisture and shear: manage incontinence if needed
|
-
Comprehensive local wound care including cleansing, debridement, control of bioburden, wound moisture balance with appropriate dressings and periwound skin protection
- If ulcer probes to the bone, evaluate for osteomyelitis
- Consider surgical reconstruction with flaps if ulcer is large, if important anatomical structures are exposed (e.g., vessels, tendon, nerves), or if osteomyelitis is present
-
Consider use of adjunctive therapy
- See section 'Diagnosis - Infection associated with PU/PI' in topic "Pressure Ulcers/Injuries - Introduction and Assessment"
|
|
Unstageable PU/PI
(Obscured full-thickness skin and tissue loss, extent cannot be determined due to presence of slough and/or eschar)
|
-
Manage underlying causes
-
Pressure redistribution: Assess need for support surface. See Stages 3 or 4 PU/PI. May may use group 2 support surfaces (powered air flotation beds, powered pressure reducing air mattresses, non-powered advanced pressure reducing mattresses).
-
Reposition patient and encourage mobility, if not contraindicated
- Optimize nutrition
- Address excessive moisture and shear: manage incontinence if needed
|
Conduct debridement: stage can only be determined when enough slough and/or eschar is removed to expose the anatomic depth of soft tissue damage involved
|
|
Deep tissue injury
(Intact or non-intact skin with non-blanchable maroon/purple discoloration or a blood-filled blister)
|
-
Manage underlying causes
-
Pressure redistribution: See Stages 3 and 4 above
-
Reposition patient and encourage mobility, if not contraindicated
- Optimize nutrition
- Address excessive moisture and shear: manage incontinence if needed
|
- Protect affected skin with moisture barrier products and skin protectants
- DTI can quickly evolve to Stage 3 or 4 PU/PI despite adequate care. If this evolvement occurs, PU/PI should be managed as Stage 3 or 4 accordingly
- There are anecdotal data on the use of non-contact low frequency ultrasound for deep tissue injury [12][13]
|
Treat the cause
For all PU/PI patients (with healable, non-healable or maintenance PU/PI):
- Ensure adequate pressure redistribution on bed and seating surface: assess need for a new support surface to reduce the forces of pressure and shear against the patient's body. Select support surfaces according to individual needs/resources and care setting
- Reposition patient to relief pressure and encourage mobility, if not contraindicated
- Optimize nutrition: in order to satisfy the individual's requirements for calories, protein, fluid, vitamins and minerals
- Manage excessive moisture and shear: manage fecal/urinary incontinence to decrease risks of skin damage and development of PU/PI and/or infection
- Address factors that can affect wound healing, to promote healing of existing PUs/PIs and to prevent new or recurring ulcers (e.g., medications, support at home, co-morbidities such as diabetes, auto-immune diseases, etc). See 'Risk Factors' and 'History' in "Pressure Ulcers/Injuries - Introduction and Assessment".
- If ulcer is of mixed etiology, manage causes of the other conditions as well
Details and evidence on interventions to treat the causes are listed below:
Pressure Redistribution
- Pressure redistribution is one of the cornerstones in management of PU/PI, as it addresses the events leading to a PU/PI.
- According to a recent PU/PI conceptual framework, PUs/PIs develop as a result of an imbalance between an individual's tolerance to external mechanical loads and mechanical loads that exceed this tolerance.[14][11] When the damage threshold of an individual is reached, a series of events occur and result in tissue damage.[14] These events include tissue deformation and decreased local blood flow, which occurs when the applied external mechanical pressure is higher than the normal arterial capillary pressure of 32 mmHg. Duration of external pressure also contributes towards local changes resulting in tissue ischemia and necrosis.[10] See section 'Pathophysiology' in "Pressure Ulcers/Injuries - Introduction and Assessment".
- The term "pressure redistribution" was coined by the NPUAP in an effort to clarify and standardize the terminology around support surfaces.[7][15] Previously known as "pressure relief" or "pressure reduction", pressure redistribution more clearly implies that to reduce pressure the area of the body in contact with the support surface can either[15][16]:
- Be increased: through immersion and envelopment by a support surface
- Be temporarily changed: through mechanically alternating the pressure beneath the body to reduce the duration of the applied pressure
- Be increased and temporarily changed by a combination of the above
SUPPORT SURFACES
-
Definition: Support surfaces are defined as “specialized devices for pressure redistribution designed for management of tissue loads, microclimate (temperature and humidity), and/or other therapeutic functions (i.e., any mattress, integrated bed system, mattress replacement, overlay, or seat cushion, or seat cushion overlay)”.[6] The goal of using a support surface is to reduce the forces of pressure and shear against the patient's body.[7]
- Types: Support surfaces have been categorized in various ways, including:
-
-
Reactive or active: A reactive support surface is a powered or non powered support surface with the capability to change its load distribution properties only in response to applied load. An active powered support surface has the capability to change its load distribution properties, with or without applied load.[17]
-
High specification: foam mattresses that relieve pressure via optimum patient immersion and envelopment while enabling patient position changes [18]
-
High tech/Low tech: Low-tech support surfaces include mattresses filled with foam, fluid, beads or air, alternative foam mattresses and overlays. High-tech support surfaces include mattresses and overlays that are electrically powered to alternate the pressure within the surface, beds that are powered to have air mechanically circulated within them, and low-air-loss beds that contain warm air moving within pockets inside the bed. Other support surfaces include sheepskins, cushions and operating table overlays. [19]
-
Groups 1,2,3: used in the United States by Medicare for patients treated at home (i.e., outpatient, home health). Groups 1 and 2 support surfaces are generally designed to either replace a standard hospital or home mattress or as an overlay placed on top of a standard hospital or home mattress [20][21][22][23]:
-
- Group 1 support surfaces: include mattresses, pressure pads, and powered pressure reducing mattress overlays (foam, air, water, or gel) (HCPCS E0181-E0189, E0196-E0199, and A4640).
- Group 2 support surfaces: include powered air flotation beds, powered pressure reducing air mattresses, and non-powered advanced pressure reducing mattresses (HCPCS E0193, E0277, E0371-E0373)
- Group 3 support surfaces: are complete bed systems, known as air-fluidized beds, which use the circulation of filtered air through silicone beads (HCPCS E0194)
Indications for support surfaces
-
1CFor all PU/PI patients (healable, non-healable, maintenance), clinical guidelines recommend support surfaces that meet individual needs and are compatible with the care setting to promote PU/PI healing. (Grade 1C) [7][6][8]
-
-
Rationale: Literature is in agreement that support surfaces are effective in preventing and treating PU/PU.[24] However, while there is moderate certainty evidence support surfaces reduce incidence of PU/PI compared with standard hospital surfaces [16], a recent meta-analysis[19] concluded that it is still unclear whether any particular type of support surface is more effective in treating PU/PI compared with standard support surfaces. In addition, there is no conclusive evidence on the superiority of any support surface. [25] Overall quality of current evidence is low/ very low (evidence level C) due to the fact that studies so far have included only a small number of participants, did not provide adequate information on their results, or were not well designed.[19] Support surfaces aim to reduce the magnitude and/or duration of pressure between patients and their support surface (i.e, “interface pressure”), thereby redistributing pressure. These devices are covered under the Medicare Durable Medical Equipment benefit for treating or preventing PU/PI benefit provided requirements are met.[20][21][22]
- Of note, critical thinking is needed when deciding if a patient with PU/PI needs a support surface. For instance, patients with a Braden score less than 18 and a PU/PI on the trunk/pelvis who can turn side to side would be able to stay on their current bed/mattress. However, if these patients cannot be turned to one side due to co-morbidities, they would need to be moved to a higher-level support surface because they have only one available turning surface.[26][27] The NPUAP/EPUAP/PPPI suggest clinicians consider replacing a patient's current mattress with a support surface if the patient [6]:
-
- cannot be positioned off the existing PU/PI
- has pressure ulcers on two or more turning surfaces (e.g. the sacrum and trochanter) that limit turning options
- fails to heal or demonstrates ulcer deterioration despite appropriate comprehensive care
- is at high risk for additional PUs/PIs; and/or
- ‘bottoms out’ on the existing support surface
Selecting support surfaces
-
Mattress/ bed: When selecting a mattress and bed support surface, the NPUAP/EPUAP/PPPI recommend consideration of the following factors [6]:
-
- Individual needs:
-
- level of immobility and inactivity;
- need for microclimate control and shear reduction;
- size and weight of the individual;
- risk for development of new pressure ulcers;
- number, severity, and location of existing PUs/PIs;
- patient safety
- Care setting:
-
- weight of the bed,
- the structure of the building,
- the width of doors,
- the availability of uninterrupted electrical power,
- and safe location for the pump/motor, including its ventilation. Plans should be in place for the contingency of power failure.
- To help identify the appropriate support surface (i.e., overlay, mattress, integrated bed system) for adults (=16 years of age) and bariatric patients in care settings where the length of stay is 24 hours or more, clinicians can use the WOCN Society's Evidence-and Consensus-Based Support Surface Algorithm. [26][27]
-
Seating support surfaces: Sitting on wheelchairs is not recommended for patients with a Stage 4 PU/PI. For other patients, if a patient with PU/PI needs to be in a sitting position, wheelchairs and seating support surfaces should be chosen after a seating evaluation. [28][6]
- Professionals involved in seating evaluations vary according to the complexity of the patient's condition, insurance coverage and availability, and may include: physiatrist, rehabilitation technology specialist (RTS) who distributes the recommended equipment, physical therapist (PT), occupational therapist (OT), rehabilitation engineer.[28][6][29] In the U.S., Medicare coverage requirements for a rehab-level power wheelchair includes a seating evaluation performed by a RTS certified as a Assistive Technology Provider (ATP). The ATP certificate can be granted to RTS, PT and OT by the Rehabilitation Engineering and Assistive Technology Society of North America (RESNA).[28] Preferably, RTS, PT and OT involved in seating evaluations should also be certified as a Seating and Mobility Specialist (SMS) by the RESNA (Medicare currently does not require that seating evaluations be performed by SMS certificate holders).[28] ATP and SMS-certified professionals can be found on the RESNA directory.
- Pressure mapping to assess interface pressures for the same individual across different support surfaces may be incorporated into the assessment.[28][10] (Figure 1)
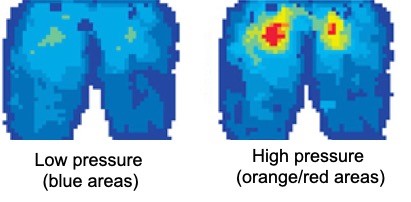
Figure 1. Pressure mapping illustrating pressure exerted on buttocks for the same individual across two different support surfaces. On the left: low interface pressure. On the right, high interface pressure
- When selecting a cushion and cover to help promote healing or prevent PUs/PIs, the following principles are helpful:
-
- Select a cushion and cover that permit air exchange to minimize temperature and moisture at the buttock interface, and that effectively redistributes the pressure away from the pressure ulcer.[6]
- If patient is capable of independent repositioning, cushion/ cover should foster independent repositioning by the patient.[9]
- Avoid using donut-type devices, as these can increase venous congestion and edema.[7]
- For Medicare beneficiaries with PU/PI who have a manual wheelchair or a power wheelchair with a sling/solid seat/back, the following seats are covered:
-
-
Adjustable skin protection seat cushion (HCPCS E2622, E2623): is covered for patients with current or past history of PU/PI.[30]
-
Combination skin protection and positioning seat cushion (E2607, E2624, E2625): is covered for patients with current PU/PI and another condition that meets eligibility criteria for a positioning seat cushion (specific ICD-10 are listed in the Medicare Administrative Contractors' Local Coverage Determination).[30]
-
Custom fabricated seat cushion (E2609): covered if patient meets criteria for either an adjustable skin protection seat cushion or a combination skin protection and positioning seat cushion and a physical therapist (PT) or occupational therapist (OT) clearly explains why a prefabricated seating system is not sufficient to meet the beneficiary’s seating and positioning needs.[30]
-
Transfers and transitions to various surfaces: Ensure transfers at the patient's environment are smooth and free of harmful pressure and shear.[9][10]
-
- A PT/OT functional evaluation of the patient in his/her environment helps assess and alleviate potential barriers to healing. For instance, patients may be able to demonstrate adequate transfer from a wheelchair to a commode at the hospital, but at home, patients may need to scoot across a room to get to the toilet because the wheelchair does not fit in the bathroom.[10] Adequate transfer techniques, transfer devices (e.g., mechanical or ceiling lifts) and repositioning equipment (e.g., low friction sheets) can help ensure adequate transfers.[9] r
For patients with a Stage 1 or 2 PU/PI
-
Mattress/ bed: Consider using a high specification reactive foam mattress or non-powered pressure redistribution support surface[6], especially if patient is able to reposition him/herself independently.[9]
-
-
For Medicare beneficiaries treated at home [20][21][22][23]:
-
- Group 1 support surfaces: covered for patients with any stage PU/PI, with a comprehensive care plan, with at least one of the following conditions: impaired nutritional status, fecal or urinary incontinence, altered sensory perception, or compromised circulatory status.
- Group 2 support surfaces (includes powered air-mattresses): covered for patients with multiple Stage 2 PU/PI on the trunk or pelvis, who over the past month have been on a comprehensive PU/PI treatment program, but whose ulcers worsened or remained the same. Documentation of comprehensive treatment should include:
-
- Use of an appropriate group 1 support surface
- Regular assessment by a nurse, physician, or other licensed health care practitioner
- Appropriate turning and positioning
- Appropriate wound care
- Appropriate management of moisture/incontinence
- Nutritional assessment and intervention consistent with the overall plan of care
- Seating support surfaces: see 'Seating support surfaces' above
For patients with a Stage 3, 4 or unstageable PU/PI
-
Mattress/ bed: Consider using a support surface that provides enhanced pressure redistribution, shear reduction, and microclimate (humidity and moisture) control. There is insufficient evidence on which to base definitive recommendations for using one surface over another.[19][6]
-
For Medicare beneficiaries treated at home [20][21][21][22]:
-
- Group 1 support surfaces: covered for patients with any stage PU/PI with a comprehensive care plan and at least one of the following conditions: impaired nutritional status, urinary or fecal incontinence, altered sensory perception, or compromised circulatory status.
- Group 2 support surfaces (includes powered air-mattresses): covered if: a) the patient has large or multiple stage 3 or 4 PUs/PIs on the trunk or pelvis, or b) if he or she has had a myocutaneous flap or skin graft for a PU/PI on the trunk or pelvis within the past 60 days and has been on a group 2 or 3 support surface immediately prior to discharge from a hospital or nursing facility within the past 30 days
- Group 3 support surfaces: covered if the patient has a stage 3 or stage 4 PU/PI and all the following conditions are met: patient is bedridden or chair-bound, would be institutionalized without the use of the group 3 support surface, the patient is under the close supervision of the patient’s treating physician, at least one (1) month of conservative treatment has been administered (including the use of a group 2 support surface), a caregiver is available and willing to assist with patient care, and all other alternative equipment has been considered and ruled out. Some manufacturers will not rent air fluidized beds for use in the home setting, so clinicians should check with the manufacturer first.
-
Seating support surfaces: For patients with a Stage 4 PU/PI, sitting on wheelchair is not recommended, except for emergencies or important issues. See 'Seating support surfaces' above
Deep tissue injury
-
Mattress/ bed: if pressure over the affected area cannot be relieved by repositioning, follow NPUAP/EPUAP/PPPI's suggestions above for pressure redistribution of a Stage 3 or 4 PU/PI.[6] Offloading and pressure redistribution may limit the extent of tissue damage. Once the ulcer has fully evolved, support surface needs can be re-evaluated.[6]
(Re)Positioning
Repositioning (i.e, changing the patient's position on a bed or seating surface) allows for relief of pressure on an existing PU/PI and on areas where PU/PI can develop. Frequency of repositioning is tailored to each individual. For patients who can reposition themselves, reminders (e.g., alarm clocks, apps) to prompt them to reposition can be helpful. Patients who cannot reposition themselves need assistance from trained healthcare professionals and caregivers. Repositioning/turning systems have been developed to help clinicians reposition patients more easily. Clinicians should avoid positioning patients on their ulcers and bony prominences. Details on repositioning frequency and techniques are described below:
-
1CClinical guidelines recommend repositioning individuals regularly to promote PU/PI healing, unless contraindicated (Grade 1C)
-
-
Rationale: literature lacks randomized controlled trials (RCTs) that address the question of whether repositioning patients improves PU/PI healing rates.[31] Despite absence of strong evidence, clinical guidelines [6][7][8] advocate for patient repositioning to promote healing of PUs/PIs. Weight bearing directly onto an existing PU/PI causes further damage due to tissue deformation and leads to decreased blood flow to the PU/PI.[31][32] Therefore, it is reasonable to suggest that individuals with PUs/PIs be frequently repositioned, to avoid depriving the wounded area of oxygen and nutrients needed for tissue repair.[31] Clinicians should avoid positioning patients on their PU/PI and bony prominences.[6][7]
- It is important to remember that there is no support surface that provides complete pressure relief.[6] Even when therapeutic support surfaces are being used, patients with PU/PI require regular turning program based on their risk level, ability to perform voluntary changes in position and contraindication to repositioning on specific areas of the body.[6][9]
-
Documentation: clinicians should strive to document every repositioning effort in the medical records in order to better coordinate care among clinicians and to fulfill legal/ethical responsibilities.[33][6] If patients refuse to be repositioned, they need to be educated on the consequences of their decision, and the education effort should be documented.
Frequency of repositioning
-
2CClinical guideline suggests clinicians create pressure relief schedules that prescribe the frequency and duration of weight shifts (Grade 2C) [6]
-
-
Rationale: Currently, there is no evidence that supports one schedule/frequency over another.[31] However, when choosing a repositioning schedule, it is important to remember that cell damage due to direct deformation damage to cells can happen in the order of tens of minutes.[34][35]
-
Use of technology to automate turning schedules: monitoring systems with sensors attached to the patient may help clinicians understand which patients need to be repositioned by staff and which patients are able to reposition themselves (see Patient Monitoring, e.g. Leaf Patient Monitoring System)
-
The exact frequency of repositioning is derived empirically, according to [7][36][6]:
-
-
The type of pressure redistribution support surface in use (e.g. high-specification foam support surfaces may allow a longer turning interval compared to standard hospital mattresses). Pressure redistribution support surfaces are costly to acquire, but are still more cost-effective than allocating more manpower for frequent turning.[36]
- Level of activity/mobility (e.g. individuals that can reposition themselves may require less frequent staff-supported repositioning)
-
Tissue tolerance, skin condition (e.g. the act of repositioning itself can create shear forces on skin, and individuals with fragile skin may not tolerate frequent turning).[11]
- General medical condition and treatment goals
- The following starting points can be adjusted to the factors above:
-
- For seated individuals: shift weight every 15 - 30 minutes
- For individuals in bed: turn according to individualized tissue tolerance, which can be as often as every 1-4 hours, unless they can reposition themselves. Inspect areas at risk at every turn.
Repositioning Techniques
Patient-centric repositioning can be guided by three principles: stability, comfort and creation of a feeling of security for the individual being repositioned.[33]
Repositioning in bed
- 2CPositions: Use the 30° tilted side-lying position (alternate right side, back, left side) or the prone position if the individual can tolerate this and her/his medical condition allows (Grade 2C)
-
-
Rationale: Studies suggest that in a 30° lateral tilt position (Figure 1), less pressure is applied on bony prominences.[36] Moreover, positioning individuals at a 30° lateral tilt has been shown to be less labor intensive and more cost-effective than positioning patients at a 90° lateral rotation (Figure 2).[36] When using the 30° lateral tilt position, positions can be alternated - right side, back, left side (Figures 1 and 3). When repositioning to the prone position, a pressure redistribution surface to offload pressure points on the face and body is recommended (Figures 4 and 5).[6] Upon each turn/repositioning, clinicians should inspect skin for additional damage and avoid positioning patients on existing PUs/PIs or on bony prominences.[6][7] Individuals who can reposition themselves are encouraged to sleep in a 30° to 40° side-lying position.[6]
- The tips below can help ensure stability, comfort and feeling of security:
-
- 30° tilted side-lying position:
-
- Make sure sacrum is off the bed. If needed, patients may be turned to a 45° tilt to offload the sacrum.[33]
- Use cushions filled with material firm enough to support the patient in position while providing comfort. Soft fill will not hold the patient in position after a short period of time, making the patient feel insecure and uncomfortable. This in turn can lead to more shear.[33]
- For hemodynamically unstable patients who cannot tolerate a 30° lateral tilt position, clinicians may opt to use a thin cushion to provide at least some lateral tilt.
- In all positions:
-
- Shoulder and pelvis should be aligned, and spine should be in a straight line. [33]
- To prevent skin damage, lift and do not drag patients.[11]
-
Turn and position systems can facilitate patient repositioning and lateral transfer by reducing the force/strain required from healthcare professionals when turning/transferring patients. Examples include Völkner® Turning System, AirTap Patient Repositioning System, Tortoise™ Positioning System, TurnAssist Patient Repositioning System, Toto® Lateral Turning System, Hercules Patient Repositioner .
- For patients with PUs/PIs on the heel:
-
- For Stage 1 or 2: to 'float the heels' off the bed, place legs on a pillow (Figure 6), or use a heel protector or suspension device that offloads the heel.[8][6] See heel protectors.
-
For Stage 3 or 4, or unstageable PU/PI: floating the heel on a pillow is not enough, PU/PI needs to be completely offloaded. Place leg or a device that elevates heel from surface of the bed and prevents foot drop.[8][6] See devices for heel offloading (e.g. Heelift® AFO and AFO Ultra, Span+Aids® Foot Drop Stop).
- 2CHead-of-bed elevation: limit head-of-bed elevation to 30° and avoid prolonged elevation unless medical conditions require otherwise (Grade 2C)
-
-
Rationale: Elevation of the head of the bed should be avoided as it produces shear forces between the skin and the bed surface, which may predispose to the development of PUs/PIs (Figure 7).[7] However, head-of-bed elevation may be medically necessary to prevent aspiration during tube feeding, to facilitate breathing in case of severe respiratory or cardiac conditions, etc.[6][7] In these cases, it is preferable that patients are positioned in the semi-Fowler's position (Figure 8) to reduce shearing forces.[6][7]
- Pressure mapping can also help in the selection of the support surface that is most appropriate for each individual. Pressure mapping may show that even when lying on a pressure redistribution support surface, when an individual has the head-of-bed elevated, pressure on the sacral area can be of 60-100 mmHg (higher than the normal capillary skin pressure of 32 mmHg).
|
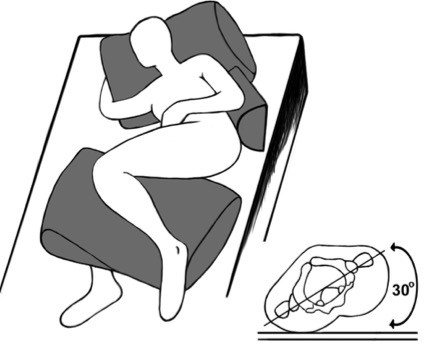
Fig.1. 30° lateral tilt position
|
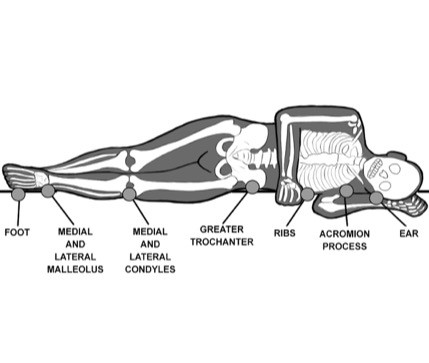
Fig.2. 90° lateral rotation
|
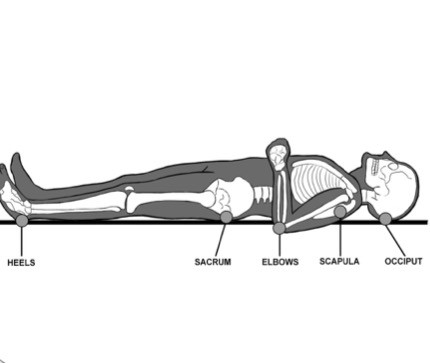
Fig.3. Supine position (back)
|
|

Fig.4. Prone position
|

Fig.5. Prone position (pressure points are offloaded)
|

Fig.6. Heel floating with a pillow
|
|
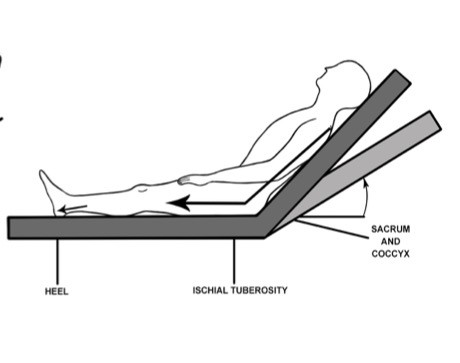
Fig.7. Shear forces resulting from head-of-bed elevation
|
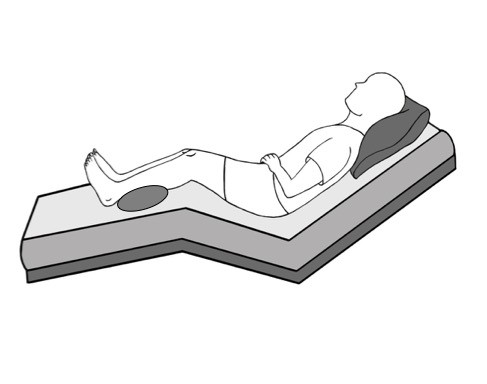
Fig.8. Semi-Fowler's position
|
|
Repositioning in seating surfaces
-
For all patients with PU/PI: minimize seating time and consult a seating specialist if PU/PI worsens.[6]
-
For patients with PU/PI in the sacrum/coccyx/ischium[6]:
-
- Consult seating specialist to prescribe an appropriate seating surface and/or positioning techniques;
- Limit sitting to 3 times a day, in periods of 60 minutes or less; with frequent pressure relieving maneuvers (e.g. wheelchair pushups) [10]
- Avoid sitting in a fully erect posture
Specific situations
-
For patients with PU/PI due to prosthetic: avoid use of the prosthetic to help promote healing, and have it refitted after PU/PI is healed to prevent recurrence [11]
- For patients in the acute hospital setting: ensure that medical devices (e.g. splints, c- collars, tubings) are removed/loosened to allow assessment of the skin, and modify them as needed and able.
Mobility
Limited mobility is an important risk factor for PU/PI development and delayed ulcer healing.[37] Thus, early involvement of PTs/OTs in the care of patients with PUs/PIs increases probability of successful healing. Therapists will evaluate patients range of motion and individual needs, and develop a plan for sitting and ambulation as rapidly as patients can tolerate.[6][9]
Nutrition
Nutrition optimization is critical for adequate wound healing. Patients at risk of or with an existing PU/PI should be screened upon admission to a healthcare facility or upon first visit in community settings by any health care team member. If the individual is at potential nutritional risk or if the individual has a PU/PI, a comprehensive nutrition by a registered dietitian should be performed.[6] It is important that a registered dietitian, together with the multi-professional care team, develop and implement a personalized nutritional plan that satisfies the individual's requirements for calories, protein, fluid, vitamins and minerals. Table 2 summarizes nutritional requirements and suggestions for PU/PI healing. For nutrition care for patients with chronic wounds, see topic " How to Screen, Assess and Manage Nutrition in Patients with Wounds".
Clinical guidelines recommendations on nutrition care for patients with PU/PI are summarized below:
-
1CClinical guidelines recommend development of an individualized nutritional plan with interventions consistent with the individual's personal goals and medical condition, to promote PU/PI healing. (Grade 1C).[38][7]
-
-
Rationale: currently, evidence regarding nutritional intervention to promote PU/PI healing is of low certainty (i.e., studies published so far have biases that do not allow for high certainty conclusions).[39][40] However, low certainty evidence should not be interpreted as nutritional interventions having no effect on PU/PI. Individuals with PU/PI require more energy/fluid intake to fuel tissue healing and compensate for liquid and protein loss through exudate. Furthermore, many patients with PU/PI do not ingest enough food/fluids due to difficulty eating, lower appetite, etc, resulting in malnutrition.[7] Despite the need for nutritional optimization, it has been shown that nutritional interventions among older patients with or at risk of PU/PI is suboptimal. In a cross-sectional study, only 25% of the patients with PU/PI were referred to a dietitian.[41] A registered dietitian, in consultation with the multi-professional care team, should develop an individualized nutritional plan to help promote PU/PI healing.[38]
- 2CFor adults who are at risk of developing a PU/PI and who are also malnourished or at risk of malnutrition, clinical guidelines suggest offering high-calorie, high-protein fortified foods and/or nutritional supplements in addition to the usual diet, if nutritional requirements cannot be achieved by normal dietary intake (Grade 2C).[38]
- 1BFor adults with a PU/PI who are malnourished or at risk of malnutrition, clinical guidelines recommend offering high calorie, high protein nutritional supplements in addition to the usual diet, if nutritional requirements cannot be achieved by normal dietary intake (Grade 1B).[38]
- 2CFor patients with a Stage 2 or greater PU/PI who are malnourished or at risk of malnutrition, clinical guidelines suggest providing high-calorie, high-protein, arginine, zinc and antioxidant oral nutritional supplements or enteral formula (Grade 2C).[38]
- Rationale: for malnourished PU/PI patients, low certainty evidence from a systematic review [40] suggests that PU/PI-specific formulas enriched with arginine, zinc and antioxidants as oral supplements for at least 8 weeks are associated with improved PU/PI healing compared with standard formulas. Arginine-enriched enteral nutrition seems to improve PU/PI healing compared with standard hospital diet as well.[42]
-
Coverage for patients with Medicare: if treated as an outpatient not receiving home health service, medical nutrition therapy (MNT) is only covered under Medicare Part B if patient has a diagnosis of renal disease or diabetes. Enteral nutrition is covered if patient has: a) permanent (lasting at least 3 months) non-function or disease of the structures that normally permit food to reach the small bowel or (b) disease of the small bowel which impairs digestion and absorption of an oral diet, either of which requires tube feedings to provide sufficient nutrients to maintain weight and strength commensurate with the beneficiary's overall health status. In the acute setting, home health and long term care, MNT is bundled in payment for the episode of care. Oral supplements/formulas are not covered. [43][44]
- For patients with PU/PI or at risk of PU/PI who cannot meet their nutritional requirements through oral intake despite nutritional interventions, clinical guidelines suggest discussing the benefits and harms of enteral or parenteral feeding to support overall health in light of preferences and goals of care.[38]
-
Table 2. Suggested nutritional optimization plan for individuals with or at risk for pressure ulcers/injuries
| Nutrients |
Suggested intake |
Adjustments/ monitoring/ comments |
| Energy (Calories) |
- 30 to 35 calories/kg body weight for adults [8][38][7]
|
- Adjust energy intake based on weight change or level of obesity [38]
- For patients with restricted special diets who do not find food palatable, revise and modify/liberalize dietary restrictions according to registered dietitian's guidance [38]
- If requirements are not achieved with regular scheduled meals, offer fortified foods and/or high calorie, high protein oral nutritional supplements between meals [38]
- Consider enteral or parenteral feeding if dietary intake continues to be inadequate, impractical or impossible [38]
|
| Protein |
- 1.25–1.5 g of protein per kg body weight
- For adults with a PU/PI Stage 3 or 4 or multiple pressure ulcers whose nutritional requirements cannot be met with traditional high calorie and protein supplements, supplement with high protein, arginine and micronutrients [38][7]
|
- Adjust protein intake based on number of ulcers, co-morbidities and renal function.[38] Individuals with kidney disease often have protein restrictions which preclude them from ingesting enough protein (monitor estimated glomerular filtration rate, normal values are greater than 60) [45] Patient with end-stage renal disease on dialysis usually do not have protein restrictions.
|
| Fluids |
- For the healing of pressure ulcers: 30–40 ml/kg or 1500 ml/day [46]
- Do not offer intravenous fluids to treat PU/PI if hydration status is adequate
|
- Adjust fluids based on co-morbid conditions (e.g., how much fluid is tolerated due to renal or cardiac diseases) and fluid losses (e.g, exudate, fever, vomiting, excessive sweating due to some pressure redistribution air and foam mattresses) [46]
-
Monitor signs/symptoms of dehydration: change in weight, skin turgor, urine output (should be at least 500 mL of urine in 24 hours), elevated serum sodium, and/or calculated serum osmolality [6]
|
| Vitamins and minerals (micronutrients) |
- Provide supplemental vitamins and minerals for patients with insufficient intake of vitamins/minerals or with identified/suspected deficit [38][8][7][47]
- Do not offer nutritional supplements to treat a PU/PI in adults whose nutritional intake is adequate.[47]
- Suggested dosing for PU/PI management, when deficiency is suspected/identified [46]:
-
- Vitamin A: For all stages of PU/PI: 10,000–50,000 IU/d orally, maximum of 25,000–50,000 IU/d, for 10–14 days at most
- Vitamin C: For PU/PI stage 1 and 2: 100–200 mg/d, for PU/PI stage 3 or 4: 1000–2000 mg/d (renal disease: adjust to 60–100 mg/d)
- Vitamin D3 (the most active vitamin D metabolite): 1000 IU/d orally. Sun exposure for 5-30 minutes between 10am to 3pm, twice a week [48]
- Zinc: For all stages of PU/PI: 220 mg/d for 10–14 days
|
- Most chronic wound patients' nutritional needs are met by educating them on how to consume a healthful diet
- Micronutrients that play a role in wound healing include vitamins A, C, D3, zinc, copper and iron [49][50]
|
Excessive moisture and shear
- Excessive moisture is a risk factor for development of PU/PI [9] and for infection of existing PU/PI. Moisture and shear can lead to the superficial breakdown of fragile skin of older individuals, contributing to the development of PU/PI. Excess moisture in the sacral area may occur due to sweat (i.e. non-breathable support surfaces), but most frequently is a result of fecal or urinary incontinence.[9]
-
- It is important to differentiate PU/PI caused by excessive moisture from incontinence-associated dermatitis. The latter is a form of contact irritant dermatitis.[9] See 'Physical Examination' in Pressure Ulcers/Injuries - Introduction and Assessment.
- Limit layers under the patient to 1 only and keep it wrinkle free. More layers can alter properties of the support surface, increase interface pressure and/or cause skin to sweat. Check with the manufacturer of the product for individual recommendations.
- For incontinent individuals, clinical guidelines recommend an individualized plan to manage excessive moisture.[8][6] The following suggestions may be considered:
-
- If episode of incontinence occurs: cleanse the skin promptly [6], apply moisture barrier products with emollients and skin protectants (e.g., made with zinc, silicone, dimethicone, cyanoacrylate) to perineal skin to protect skin from excessive moisture.
- To minimize episodes of incontinence, establish a toilet/bowel routine
- If using incontinence pads/underwear, check for soiling upon repositioning or every 4 hours if patients can reposition themselves
- For fecal incontinence in bed-bound individuals with a sacral PU/PI, consider an external or internal collection device. External devices usually do not stay in place for very long and have limited wear time (e.g., Bard Fecal Containment Device). Internal fecal containment devices are limited to liquid/ semi-liquid stool for no more than 30 days provided patient does not have contraindications (rectal bleeding, etc) (e.g., Convatec Flexi-Seal™ Protect FMS, Bard Dignishield Stool Management System). A temporary diverting colostomy is recommended when multiple PUs/PIs with proximity to the anus are present, until the ulcers are healed or surgically closed. For non bed-bound individuals ensure diet has been optimized to minimize liquid stools, which are more difficult to contain.
- For urine incontinence, external catheters may be used (e.g, Purewick® Female External Catheter, Men's Liberty). External urinary pouches may be used in obese men.
- For fungal infection associated with incontinence-associated dermatitis, the following steps may be considered [51]:
- If the individual is not immunocompromised, initiate treatment with a trial of zinc oxide and exposure to air. If no response is seen after a few days, proceed to next steps.
- Lightly dust anti-fungal powder on affected areas, seal with ointment or liquid skin barrier. If no improvement after a few days, collect skin culture using a validated technique to assess for associated bacterial infection.
- Assess for other areas that can be affected such as oral mucosa (thrush), skin folds and genitalia and treat accordingly. Oral anti-fungal treatment is recommended.
Other underlying causes if ulcer is of mixed etiology
- Address other underlying causes if the ulcer has mixed etiology. For instance, consider offloading foot if a neuropathic/neuroischemic etiology is suspected or consider compression therapy if associate chronic venous insufficiency, lymphedema are suspected. See topics "Diabetic Foot Ulcer" and "Venous ulcers".
Address patient’s concerns
For all patients (with healable, non-healable or maintenance PU/PI), concerns should be addressed and plan of care adjusted accordingly.
Pain control
- 1CIt is recommended that clinicians manage pain by addressing the underlying causes of pain and administering analgesics (Grade 1C)
-
-
Rationale: PUs/PIs are painful and this pain is often underestimated by clinicians.[6][9] Patients with spinal cord injury may still feel pain below the level of injury, and patients without spinal cord injury may report excruciating pain, discouraging them from repositioning themselves.[10] Also, increased level of pain may indicate infection and warrants investigation. Controlling pain helps promote wound healing and alleviate anxiety.[9]
- To manage pain, clinicians might opt to:
-
- Establish/follow a repositioning schedule to avoid pressure-related pain.[5] See section 'Repositioning'
- Select dressings to minimize pain: choose dressings that are non-adherent and require less frequent changing.[6] Consider hydrocolloids if PU/PI not located on trunk, hydrogels, alginates, polymeric membrane foams, foam and soft silicone dressings. Ibuprofen-impregnated dressings are not available in the U.S. but may be considered as a topic analgesic treatment for PU/PI.[6] Dressings that contain viscous lidocaine may be used (e.g, Regenecare®, WoundPal®), or lidocaine gel can be added to the dressing or to the wound.[5] See topic "Dressing Essentials"
- Provide analgesia before dressing changes, debridement and other procedures and as needed.[6] The World Health Organization (WHO) Pain Ladder for cancer patients, with modifications for wound care may be used. Benefits and harms of each step should be considered. In summary [52]:
-
- Step 1: A non-opioid analgesic (e.g., NSAID) with or without an analgesic adjuvant. Adjuvants include tricyclic antidepressants (e.g., nortriptyline starting at 10-30 mg at night), anticonvulsants (e.g., gabapentin), antihistamines, benzodiazepines, steroids, and phenothiazines.
- Step 2: If pain is not controlled: Continue the initial medication and add an opioid, such as codeine or tramadol, and an adjuvant
- Step 3: If pain is not controlled: Discontinue second step medications and initiate a more potent oral narcotic
Depression
-
For all patients with PU/PI, it is recommended that a psychologist/ mental health professional be involved at the earliest stage possible in the treatment process, preferably in clinic prior to admission to the acute care setting.[10]
-
-
Rationale: Depression has been shown to be highly prevalent among elderly individuals with PU/PI living in their community.[53] It has been shown that depression adversely affects potential for wound healing.[54] Also, depression is associated with decreased mobility, which leads to development or delay in healing of PU/PI.[10] Limited mobility can lead to depression or depression can lead to limited mobility.[10] Individuals should be encourage to engage in their daily activities as much and as soon as possible.
Odor
- Malodor is usually caused by a combination of necrotic tissue, infection, and excessive exudate. Poor general hygiene and dressings left on for too long may contribute to malodor as well. [55]
- For odor control, presence of necrotic tissue and infection should be assessed and addressed first:
- Necrotic tissue: should be debrided as indicated, as it serves as a substrate for bacterial growth. See section 'Debridement' below.
- Infection: malodor is often a result of infection with anaerobic bacteria. After debridement, wound culture should be obtained with a validated method. If signs of local infection, topical antibiotic therapy should be initiated. If signs of spreading or systemic infection, topical and empiric systemic antibiotics should be initiated. If culture indicates presence of anaerobic bacterial, oral metronidazole should be initiated. Topical antimicrobials for malodorous wounds include topical metronidazole, silver sulfadiazine, preparations containing neomycin, bacitracin and polymyxin B, medical grade honey, PHMB dressings. [55][56]
-
-
Topical metronidazole: 0.75% or 0.8% gel can be applied directly on the wound once or twice daily for 7 days to reduce odor.[56] Crushed tablets can also be used [5] (authors' experience is that 500 mg can be crushed into a fine powder and sprinkled on to the wound after irrigating the area with either 0.25% acetic acid or 0.025% Dakin's solution). Small size RCTs have shown that topical metronidazole is more effective than placebo [57][58][59] and as effective as 0.2% polyhexamethylene biguanide (PHMB) in reducing chronic ulcer malodor.[60] A systematic review concluded that current evidence derived from these small RCTs is of low certainty and thus not strong enough to recommend routine inclusion in guidelines.[61] Topical metronidazole may control odor through its action on anaerobic bacteria that produce volatile acids, without the side effects of oral use as there is little or no systemic absorption. In a large, international survey (n=1444 clinicians) on interventions to control ulcer odor, metronidazole was used by only 43% of the respondents, however among those who used it 49.8% considered it very effective.[62] Reasons behind the relatively low adoption could be lack of availability in some countries, cost and need for prescription. In the U.S., use of topical metronidazol for ulcer malodor is off-label.
- Acetic acid: a sweet odor, blue-green drainage, and wet yellow slough are characteristic signs of infection with Pseudomonas aeruginosa, an aerobic organism. In these cases, clinicians may opt to apply gauze moistened with 0.25% acetic acid twice daily until healthy granulation tissue forms.[63][64]
- To manage exudate: use of dressings with higher absorption capacity is recommended, with or without activated charcoal or sodium chloride.[55] See topic "Dressing Essentials"
- Odor concealers: may be use as adjuncts to the interventions above, however adjuncts alone will not stop ulcer from having a foul odor. These include adsorbents (e.g., charcoal), kitty litter/ground coffee under the bed, commercial deodorizers and peppermint oils on dressings.
- Charcoal dressings: a systematic review found that activated charcoal dressings applied to fungating wounds significantly controls odor, as long as the dressing is sealed and the wound is dry.[65] Examples include CarboFLEX (ConvaTec, USA), Clinisorb (CliniMed Ltd., UK), Actisorb Silver (KCI, an Acelity company, USA).[56] In a large, international survey (n=1444 clinicians) on interventions to control ulcer odor, charcoal dressings was the most used intervention, however only 48.4% rated this as being very effective.[62] This may be due in part to the wide range of products available, with different modes of action and application methods.
Local Wound Care
For all patients (healable, non-healable, maintenance), appropriate local wound care should be implemented. Table 3 summarizes local wound care interventions for healable and non-healable/maintenance PU/PI.[2][3][6][9]
Evidence and recommendation for each intervention are listed after the table. For customized, wound-specific recommendations, use Wound Prep and Dress Tool.
Table 3. Local wound care for pressure ulcers/injuries
|
Healable |
Non-healable/ maintenance |
| Cleansing |
- Gently cleanse with sterile saline, water, 0.5-1% acetic acid, or wound cleanser
- If solution cannot be retrieved/aspirated (due to undermining, sinuses, etc), use forceps to hold moistened gauze ribbons and cleanse the wound. Ensure all gauze is retrieved
|
- Keep wound bed dry
- May cleanse ulcers with antiseptic agents to help manage bioburden, odor and moisture
|
| Debridement |
- Stage 1 and 2 PU/PI: debridement not indicated
- Stages 3 and 4 PU/PI, unstageable PU/PI due to slough/eschar: debridement indicated for removal of devitalized tissue at initial assessment and on a regular basis until wound bed is covered with granulation tissue; for wounds with no signs of improvement despite standard care for 2 - 4 weeks; and for infected wounds.
- For ulcer in lower extremity, perform thorough vascular assessment to determine if blood supply is sufficient to support healing of the debrided wound
- If dry eschar in ischemic limb: do not debride; monitor for signs of infection
- Choice of debridement methods:
-
- Choice depends on patient condition and resources (clinician's skills, license restrictions, resources available).
- For PU/PI with extensive necrosis, Stage 3 or 4 with undermining, sinus tracts or signs of infection (i.e. advancing cellulitis, crepitus, fluctuance, and/or sepsis secondary to ulcer-related infection): initial surgical debridement in the operating room is recommended
- If there is no urgent clinical need for drainage or removal of devitalized tissue: sharp conservative, mechanical, enzymatic, autolytic and/or biological debridement may be used
- Sensate patients may not tolerate sharp debridement at the bed side and may need to be debrided in the operating room
|
- For dry, stable eschars without fluctuance or erythema: do not debride
- For Stage 1 and 2: do not debride
- For Stage 3 and 4 PUs/PIs: conservative debridement of nonviable tissue only
- For PU/PI with extensive necrosis or signs of infection (i.e. advancing cellulitis, crepitus, fluctuance, and/or sepsis secondary to ulcer-related infection): initial surgical debridement in the operating room may be considered if this intervention is aligned with the patient's and caregiver's goals
|
| Infection and bioburden control |
- If no signs of infection, do not use antimicrobial dressings
- If clinical signs of local infection or no healing is seen within 2 weeks of debridement and pressure redistribution, collect wound culture post debridement and initiate topical antimicrobials
- If spreading or systemic infection, collect wound culture post debridement and initiate systemic antibiotics and topical antimicrobials
- Antimicrobial dressings (with PHMB, cadexomer iodine, silver sulfadiazine, other silver products, honey):
-
- For light exudate: hydrogel, or hydrogel colloidal sheet-based
- For moderate/heavy exudate: Alginate, fiber gelling dressing (hydrofiber), specialty absorptive
- Osteomyelitis should be considered if ulcer probes to bone
|
- If clinical signs of local infection, collect wound culture post debridement or gentle removal of necrotic tissue and initiate topical antimicrobials
- If spreading or systemic infection, collect wound culture post debridement or gentle removal of necrotic tissue and initiate systemic antibiotics and topical antimicrobials
- Topic antimicrobials:
-
- If minimal/ light exudate, consider painting wound with antiseptic solution or using a topical antimicrobial agent
- If moderate or heavy exudate, consider non-adherent antimicrobial dressings (with silver, cadexomer iodine, medical-grade honey, silver, etc):
- Osteomyelitis should be considered if ulcer probes to bone
|
| Peri-wound skin care |
- If excessive exudate: use zinc, dimethicone, silicone-based skin protectant, or skin prep to protect periwound
- If dry skin use moisturizer with humectants for skin hydration
|
| Moisture balance |
- Dressing choice depends on ulcer characteristics, clinical experience, patient preference, care setting and cost.
- Maintain wound moisture or provide moisture to dry wounds with:
-
-
Hydrocolloid, hydrogel, foam dressings, honey gel
- Manage exudate with:
-
-
Alginate, fiber gelling dressing (hydrofiber), foam dressings, composite, specialty absorptive
- Fill deep wounds to avoid dead space. Do not pack wounds tightly
- See Wound Prep and Dress Tool, WoundReference's Dressing Feature Matrices
|
- Keep wound dry.
- If exudate: apply appropriate non-adherent dressing
- Fill deep wounds to avoid dead space. Do not pack wounds tightly
- Avoid conventional dressing products that require daily dressing changes. See Wound Prep and Dress Tool, WoundReference's Dressing Feature Matrices
|
Cleansing
-
2CFor healable PUs/PIs, clinical guidelines suggest cleansing with a pH-balanced, non-irritating, non-toxic solution (e.g. tap/sterile water, saline, wound cleanser) prior to each dressing change (Grade 2C)
-
-
Rationale: To date, no RCT has evaluated the effect of PU/PI cleansing compared with no cleansing to promote wound healing. [7] [66] There is no strong evidence supporting use of one cleansing solution or one irrigation pressure level over another.[66] A few small trials with biased design have found low certainty evidence that some cleansing methods/solutions were superior to control (i.e., saline spray with Aloe vera, silver chloride and decyl glucoside better than saline; pulsatile lavage better than no cleansing).[66] However evidence is still insufficient to recommend one intervention over another. Yet, cleansing removes debris that can interfere with healing and thus guidelines recommend cleansing prior to each dressing change with water, saline or wound cleanser. Cleansing healable ulcers with antiseptics is not recommended, as they are toxic to granulation tissue.[7]
- Below are a few best practices, based on clinical experience and expert opinion:
-
- A cost-effective option is to use mild, neutral, non-scented, no residue soap (e.g, liquid soap) and water. Tap water from a reliable source does not increase infection rate [7]
- Do not irrigate ulcer with pressure so strong that it damages tissue.
- Cleanse the periwound as well, and ensure irrigated solution that spills/flow out of the wound does not re-enter it to minimize contamination
- If solution cannot be retrieved/aspirated (due to undermining, sinuses, etc), use forceps to hold moistened gauze ribbons and cleanse the wound. Ensure all gauze is retrieved.
- For patients with Medicare being treated as an outpatient, Medicare part B does not cover commercial cleansers.
- For non-healable/maintenance PUs/PIs or for infected ulcers, clinicians might opt to cleanse ulcers with antiseptic agents to help manage bioburden, odor and moisture (Grade 2C)
-
-
Rationale: Wound antiseptics may be used for cleansing wounds that have are not likely to heal or for infected PUs/PIs.[6][7] Some considerations to keep in mind [6]:
-
- Dakin's solution at concentrations lower than 0.025% or hypochlorous acid may be viable options
- Hydrogen peroxide should be avoided as it is highly toxic even at low concentrations
- Iodine products should be avoided in patients with renal failure, iodine sensitivity and thyroid disorders. Povidone-iodine (PVP-I) is not recommended for ulcers with healing potential (healable ulcers) as it reduces moisture and can be toxic to cells important in the wound healing process. [67]
- For patients with Medicare being treated as an outpatient, Medicare part B does not cover commercial cleansers.
Debridement
-
For healable, Stage 2 - 4 PUs/PIs, we recommend debridement over no debridement of devitalized tissue to promote wound healing, when aligned with goals of therapy and not contraindicated (Grade 1C)
-
-
Clinical guidelines [6][7][8][47] recommend debridement of devitalized tissue (e.g. fibrin, eschar, debris, necrotic tissue) to promote healing of PUs/PIs, despite lack of studies comparing debridement with no debridement. Debridement has many benefits: it removes devitalized tissue, which interferes with wound healing and facilitates bacterial growth, allows staging of the ulcer, and enables collection of adequate culture samples. Furthermore, Medicare part B will only cover surgical dressings for ulcers that have been debrided or surgically created.[68] Topical anesthetics may be used prior to conservative debridement procedures.
Indications
- If devitalized tissue is present, debridement can be performed at initial assessment and on a regular basis, until wound bed is covered with granulation tissue.[6][7] Maintenance debridement is needed as other necrotic areas can become apparent later.
- For non-healing ulcers (i.e., no signs of improvement in four weeks or more of standard wound care): sharp and/or mechanical debridement is indicated for removal of biofilm, which may contribute to delayed healing [6][69][70]
- PU/PI with ulcer-related spreading or systemic infection (i.e., cellulitis, crepitus, fluctuance, and/or sepsis) should be surgically debrided.[6]
Caution
-
For PU/PI in lower extremities: do not debride ulcer if blood supply to the wound is not adequate enough to support healing post debridement.[6] A thorough vascular assessment prior to debridement should be performed. See table with values and interpretations of non-invasive arterial tests in topic "How to Select Adequate Compression Therapy Pressure Levels and Products".
-
PU/PI in ischemic limb, covered with stable, hard, dry eschar should not be debrided.[6][8] At each dressing change, eschars should be monitored for signs of developing infection, which include: erythema, tenderness, edema, pus, fluctuance, crepitus and/or malodor.[6] Should any of these signs be identified consult a vascular surgeon, as urgent PU/PI debridement is indicated.[6]
-
For PU/PI in heel with adequate blood supply: heel ulcers with no signs of inflammation/infection and with stable, dry eschar do not need debridement.[7] If performed, debridement should be done with care, as there is little subcutaneous tissue under the eschar in this region.[11]
-
For PU/PI covered with dry eschar regardless of region: if no purulence, fluctuance or erythema, the eschar may be left in place so that tissue underneath can heal on its own, based on clinical judgement.[11]
- For non-healable or maintenance wounds, guidelines recommend against active aggressive debridement.[8][6]Aggressive debridement without adequate blood supply and immune defense may increase risk of infection (especially if the wound bed is excessively moist) and increase size of a wound that is already difficult to heal. Instead, these wounds should be kept dry, and necrotic tissue may be carefully removed.
debridement techniques
-
As for choice of debridement for healable PUs/PIs, clinicians can opt from several methods (e.g., surgical, sharp, mechanical - including ultrasound and hydrosurgical, enzymatic, autolytic, biologic) according to patient's condition, wound bed, resources and clinical setting. (Grade 2C) [6][7]
-
- Rationale: When choosing debridement methods, it is important that clinicians take into account relative contraindications such as use of anticoagulants, presence of severe ischemia, clinical context, availability of expertise and supplies, patient tolerance and preference, cost-effectiveness, professional licensing restrictions and insurance coverage. There are no studies to date supporting significant evidence of one debridement method over another. Therefore, choice of debridement method should be at the clinician’s and patient’s preference.
- The following guidelines may be helpful:
-
- For PU/PI with extensive necrosis, Stage 3 or 4 with undermining, sinus tracts or signs of infection (i.e. advancing cellulitis, crepitus, fluctuance, and/or sepsis secondary to ulcer-related infection): initial surgical debridement in the operating room is recommended to provide a more definitive procedure. [11][6]
-
If there is no urgent clinical need for drainage or removal of devitalized tissue, conservative sharp, mechanical, enzymatic, autolytic and/or biological debridement may be used[6]
- In patients with spinal cord injury sharp debridement may be done at the bed-side, whereas for sensate patients debridement in the operating room may be needed.
-
Conservative sharp debridement (Figures 9-13): It must be performed by trained, licensed healthcare practitioners. It is performed with sterile curettes, scissors, scalpels, forceps at bedside or procedure room. Caution should be exercised in the presence of immune incompetence, compromised vascular supply, bleeding disorders or use of anticoagulants.[6][8]The patient/caregiver should be forewarned that bleeding is likely and that the wound will appear larger after the procedure. This method does not have the extra risks associated with general/regional anesthesia and costs of surgical facilities. It is less aggressive than surgical debridement and is fast, but may also be imprecise and may carry the greatest risk of tissue damage of any of the debridement methods.[71] See topic "How to Perform Conservative Sharp Wound Debridement".
-
Surgical debridement: performed in the operating room, under anesthesia. Indicated if fast and effective removal of large amounts of necrosis is the goal. Contraindicated if trained/licensed professional and resources are not available, if vascular supply to the wound is inadequate and if sepsis without systemic antibacterial coverage.[7] Relative contraindications include bleeding disorders and anticoagulation.[7]
-
Mechanical debridement: includes physical mechanical removal of devitalized tissue through wet-to-dry dressings, brushes, wound irrigation, ultrasonic debridement with contact low frequency (22.5, 25 or 35 kHz) ultrasound (e.g, Versajet, Qoustic Wound Therapy System™). Wet-to-dry dressings can be painful and can damage new tissue upon removal if dry. Irrigation with pulsed lavage may effectively remove loose necrotic tissue at pressures ranging from 4-15psi.[7]
-
Enzymatic debridement: collagenase may be applied on non-infected PU/PI at a thickness of ~2mm daily and covered with a non-adherent dressing.[72] Moisture is needed to optimize effects. If wound bed is dry, cover with a damp saline gauze or petrolatum. Collagenase should not be used with products that inhibit its activity, including certain silver products. See interactive topic "Products that inhibit collagenase enzymatic activity"
-
Autolytic debridement: not indicated for ulcers with signs/potential for infection or ischemia, or for very deep wound that requires packing.[7] Uses occlusive dressings (e.g. hydrogels, hydrocolloid) to create a moist wound environment in which exudate and endogenous enzymes liquefy slough and promote granulation.[7] This method is slow and needs exudate but it is highly selective, painless and requires only minimal clinical training.[73] Moisture-donating dressings can predispose to periwound skin maceration. If there are no signs of tissue autolysis in 1-2 weeks, it is advisable to select another debridement method.[7]
-
Biological debridement (e.g, maggots): consists in applying irradiated maggots on the wound, so that they can eat and degrade the necrotic tissue.[7] Larval therapy provides both debridement and antibacterial activity.[7] It is not indicated for patients with personal bias against maggots, in the presence of active hemorrhage or bleeding disorders, exposed blood vessels, limb or life-threatening infection, necrotic bones or tendons, inadequate perfusion for healing, wounds in deep cavities or sinus tracts of unknown origin, rapidly advancing tissue necrosis, and/or allergy/sensitivity to larval proteins or the nutrient media for the larvae.[8]

Fig.9. Unstageable PU/PI on right heel | 
Fig.10. After conservative sharp wound debridement (CSWD)- stage 3 PU/PI | 
Fig.11. 4 weeks after CSWD and appropriate treatment -decrease in wound size |

Fig.12. 8 weeks after CSWD and appropriate treatment - wound epithelialization | 
Fig.13. 10 weeks after CSWD and appropriate treatment - further epithelialization and healing |
|
Infection and bioburden control
Interventions to manage PU/PI infection include debridement, topical antiseptics/antimicrobial agents, systemic antibiotics and surgical procedures.
-
In the absence of clinical signs of infection, clinical guidelines recommend against routine use of antimicrobial dressings or systemic antibiotics.[47] See clinical signs of infection in section 'Physical Examination - Infection associated with PU/PI' in topic "Pressure Ulcers/Injuries - Introduction and Assessment"
Soft tissue local infection
-
For healable, locally infected PUs/PIs (e.g, increased exudate, redness, size, pain): Debride the wound and collect wound specimen for culture and sensitivity.[7] Topical antimicrobial agents may be used (e.g., silver sulfadiazine cream and other silver products, medical-grade honey, polyhexamethylene biguanide, cadexomer iodine) until clinical signs of infection subside or while cultures show >1×10^6 cfu/gram of tissue or any tissue level of beta hemolytic streptococci.[6][7][74] Once in bacterial balance, (i.e., <10^5 cfu/gram of tissue and no beta hemolytic streptococci in the ulcer) topical antimicrobials should be discontinued to minimize possibility of emergence of resistance.[7]
-
- As for choice of topical antimicrobial to promote healing of infected or non-infected PU/PI, a comprehensive review of current evidence did not find convincing evidence that favors one antimicrobial treatment over another.[75]
-
If there are no signs of infection, but no signs of wound healing (contraction or epithelialization) within 2 weeks from debridement and adequate pressure redistribution: biofilm may be preventing wound healing (biofilm is a cluster of bacteria embedded in a matrix covering the wound).[69] Clinical guidelines and expert consensus recommend a new sharp and/or mechanical debridement and collection of post-debridement wound specimen for culture and sensitivity, topical antiseptics and/or antimicrobial agents for 2 weeks, along with maintenance debridement. [6][7][8][69][70]
-
For infected, non-healable/maintenance PU/PI: keep the ulcer dry, utilize topical antiseptic agents (e.g., Dakin's solution at concentrations lower than 0.025%) and/or antimicrobial dressings.[6][8]
ABSCESS
- Local abscess should be surgically drained.[6] Systemic antibiotics may be administered if there is associated cellulitis, or if abscess is deep or large
Systemic infection, related to the ulcer
- For healable/ non-healable/ maintenance individuals with clinical evidence of spreading or systemic infection (e.g., positive blood cultures and fever, cellulitis, fasciitis, osteomyelitis, systemic inflammatory response syndrome, or sepsis): initiate systemic antibiotics and topical antimicrobials.[6][8][47]
-
- If wound present for more than 4 weeks or if patient immunocompromised, consider coverage for gram-positive, gram-negative and anaerobic organisms.[9]
- Consult infectious disease professionals or hospital microbiology department to confirm that selected antibiotics are effective against local strains of microbes[47]
OSTEOMYELITIS
- If ulcer probes to the bone, or has not shown signs of improvement despite standard therapy, evaluate the individual for osteomyelitis. [6] See section 'Diagnosis - Infection associated with PU/PI' in topic "Pressure Ulcers/Injuries - Introduction and Assessment"
- Treatment of osteomyelitis includes debridement of devitalized/infected bone, systemic culture-guided antibiotics and definitive coverage of the wound with flaps.[7] Culture-guided antibiotic therapy is recommended for 6 weeks for most cases.[7] If MRSA is detected, antibiotic therapy should be extended to 8 weeks.[7] See section 'Surgical Reconstruction' below.
Peri-wound Care
- Excessive moisture: Protect skin with moisture barrier products based on zinc, silicone or dimethicone, and/or skin protectants based on cyanoacrylate.[6][8]Excessive moisture leads to skin damage, which can lead to development of PU/PI.[6]
Moisture management and dressing selection
- 1CFor non-infected, healable PUs/PIs, we recommend clinicians apply a topical dressing that will manage excess exudate, protect periwound skin and maintain a moist wound bed, with the least amount of dressing changes possible (Grade 1C)
-
-
Rationale: Several experimental studies support the hypothesis that a moist wound bed increases wound healing when compared to a dry wound bed, by facilitating cell migration and matrix formation.[76][77] Guidelines recommend achieving local moisture balance and exudate management.[6][7][47] Local moisture balance is necessary to facilitate granulation and reepithelization of the ulcer.[7] It has been shown that chronic wound exudate has high concentrations of proteases and inflammatory cytokines that prohibit wound healing and may damage the fragile periwound skin, and thus exudate management is also essential.[78][79][80]
- To achieve this goal, monitor and assess ulcer and modify type of dressings as ulcer changes its characteristics.[8] For instance, dry/absorptive dressings can be used in the 24 hours post-debridement to absorb bleeding, then moist dressings can be reinstituted after that.[7]
- Of note, wet-to-dry dressings are not considered continuously moist and require frequent dressing changes, which increases cost of care.[6] Caution is required with the use of occlusive moisture retaining dressings (i.e., films, hydrocolloids, acrylates), especially if infection is suspected.
-
For infected PUs/PIs: regular inspection and assessment are needed. See section on 'Infection and bioburden control'.
-
For non-healable/maintenance PUs/PIs, if minimal or no exudate, a topical antiseptic may be used.[47] If exudate management is needed, non-adherent dressings may be applied.
Dressing selection
Selection of primary and secondary dressings should follow established wound bed preparation principles. [3][2][81][10][9] For customized, wound-specific recommendations, use Wound Prep and Dress Tool. For practical information on dressing indications, contraindications, application, Medicare coverage and brands see "Dressing Essentials" and "Dressing Brands Quick Reference". General recommendations and evidence regarding dressings for PUs/PIs are listed below.
- 2CClinicians may opt to select dressings to treat PU/PI based on ulcer characteristics, clinical experience, patient preference, care setting and cost. (Grade 2C).
-
-
Rationale: current evidence is not strong enough to justify recommendation of one type of dressing over another to treat PU/PI.[82] A systematic review observed that trials in this area are generally small and at high risk of bias, thus it is unclear whether the dressings examined are more effective than saline gauze.[82]Guidelines and expert opinion recommend choice be guided by ulcer characteristics, clinical experience, patient preference, care setting and cost.[6][10][8][47]
- Wound characteristics: characteristics such as wound bed, depth, exudate should be considered when choosing dressings for PUs/PIs. Consideration should be made to change the type of dressing if the ulcer does not show signs of improvement after 2 - 4 weeks of adequate standard care. Adverse effects such as maceration, infection, or further loss of tissue should prompt a change in wound dressing as well.
- Use of resources: with respect to cost, it is important that clinicians consider not only the cost of dressings when selecting dressings, but also cost of other resources needed when utilizing each type of dressing.[7] Frequency at which manufacturers recommend dressings to be changed has a direct impact on nursing time and cost. WoundReference's Dressing Feature Matrices allow clinicians to compare frequency and other features side-by-side.
- A few considerations regarding dressing types, relevant to PUs/PIs [6][10][10]:
-
- Wet-to-dry dressings should be avoided, as dry gauze causes pain when removed, and leads to desiccation of viable tissue.[6]
- For deep ulcers: a lightly packed, single gauze strip/coarse roll (Kerlix, etc) may be used to fill the cavity. Tight packing creates pressure on the wound and prevents development of new granulation tissue. Ensure dressings are removed at every change, as retained dressings in the ulcer can serve as a source of infection. Impregnated gauze (e.g. Xeroform) can be used to cover saline dressings underneath and prevent evaporation of moisture.
- When selecting dressings, consider the support surface in use: air fluidized mattresses/beds for instance, may be filled with air and glass sand beads at up to 90 degrees Fahrenheit, and the warm air will rapidly dry moist dressings that do not have an impermeable cover.
Plan Reassessment
Plan of care should be reassessed for healable PUs/PIs that fail to show some evidence of healing progress (e.g., wound contraction, re-epithelialization) in 2 - 4 weeks of standard treatment.[6][7][4] These ulcers are also known as recalcitrant, refractory or non-healing ulcers. For details on standard treatment, see sections 'Treat the Cause', 'Address Patient's Concerns' and 'Local Wound Care' above. Healing expectations are adjusted according to presence of co-morbidities, care setting and interventions used.[6][4] As a baseline parameter, retrospective data have shown the following healing rates for PUs/PIs [83]:
- Stage 2: 7 weeks
- Stage 3: 10 weeks
- Stage 4: 19 weeks
Re-evaluation of the patient and ulcer should be performed before use of adjuvant therapies.[6][7] Re-evaluation includes assessment of differential diagnoses, factors impairing treatment of the underlying causes, reassessment of patient's concerns, adequacy of local wound care and any factors delaying resolution of infection. If after reassessment the provider decides to keep the current plan, reasons for the decision must be adequately documented to prevent medical-legal issues.[4] A checklist such as the one shown in Table 4 can be useful in reassessing plan of care:
Table 4. Checklist for reassessment of PU/PI treatment plan
| For all healable PUs/PIs: Check differential diagnoses |
- See section 'Differential Diagnosis' in "Pressure Ulcers/Injuries - Introduction and Assessment"
|
| For all healable PUs/PIs: is the cause being adequately addressed? |
- Check for adequate pressure redistribution, repositioning, transfer and plan to increase mobility
-
- Consider replacing the mattress with a support surface that provides more effective pressure redistribution, shear reduction, and microclimate control, but only if remaining standard of care interventions were adequately carried out.[6]
- Does the repositioning schedule need to be reviewed?
- Can patients adequately transfer from one surface to another at home? Patients/caregivers may believe that care setting at home is adequate, but setting should be confirmed by a PT/OT professional
- Check for adequate glycemic control and nutritional intake
- Check for adequate moisture/incontinence management
- Check for any co-factors that may be impeding healing (e.g., medications, smoking, immunosuppression, etc). See 'Ulcer healability' in "Pressure Ulcers/Injuries - Introduction and Assessment".
- Check for soft tissue infection and/or osteomyelitis
-
- Consider tissue biopsy, validated quantitative swab technique (e.g. Levine technique) or wound fluid protein analysis. For assessment and diagnosis of infected PU/PI, see section 'Infection associated with PU/PI in' "Pressure Ulcers/Injuries - Introduction and Assessment"
- Check for presence of any "acquired bursa" between the skin and underlying bone or at the base of the ulcer. For instance, anatomically, there is no ischial bursa, but one can develop due to sliding forces over that area. This bursa can delay healing and become infected. [10][84][84]
- Check for adequate vascular supply to the ulcer if it is located in the lower extremity
-
- See values of arterial non-invasive bedside tests and likely interpretation
|
For all healable PUs/PIs: are patient's concerns addressed?
|
- If patient is not adherent to treatment plan, what are the factors that prevent patient from adherence?
- Check for potential psychosocial aspects preventing healing (e.g., depression, addiction to drugs, etc)
|
For all healable PUs/PIs: is local wound care adequate?
|
- Debridement: Ensure adequate removal of devitalized tissue and surrounding callus (See section 'Debridement' above)
- Is bioburden being adequately managed?
- Dressings: Aim is to manage excess exudate, protect periwound skin and maintain a moist wound bed, with the least amount of dressing changes possible (See section 'Moisture management and dressing selection' above)
|
| For infected PUs/PIs: assess the following factors |
- Is there unidentified necrotic soft tissue or bone?
- Is there an undrained abscess?
- Is there osteomyelitis that has not yet responded?
- Is there an untreated or an unidentified pathogen?
- Is there an antibiotic delivery problem?
- Is there an antibiotic non adherence issue?
- Have all metabolic aberrations been corrected?
|
Surgical Reconstruction
Overview
Surgical consult is indicated for full thickness ulcers that are extensive or refractory, if important structures are exposed (e.g., vessels, nerve, bone, muscle, fascia) or osteomyelitis is suspected. Surgical reconstruction is often a major procedure that requires planning and adequate preparation for care before and after surgery to prevent complications and recurrence.
- 2CFor healable PUs/PIs that are: classified as Stage 3 or 4 with no signs of healing for 4 weeks despite standard care (i.e. refractory), are extensive in size or interfere with the daily life of the patient, have exposed organs/vessels or have osteomyelitis, we suggest consideration for definitive wound coverage with surgical reconstruction. (Grade 2C)
-
-
Rationale: Clinical guidelines and experts recommend a surgical consultation for consideration of surgical reconstruction for non-healing Stage 3 or 4 PUs/PIs without contraindications to surgical procedures or anesthesia.[6][7][10][85]There have been no randomized controlled trials (RCTs) studying the effectiveness of surgical reconstruction in this context.[85] Despite the lack of evidence generated by RCTs, surgery is an established modality in the treatment of refractory ulcers.[86][10][85] Definitive wound closure decreases protein and fluid loss, the risk of infection, and propensity to development of malignancy in the wound.[7] Choices on the indication for surgical reconstruction depend on availability of surgical expertise, the patient's condition, ulcer characteristics and recurrence, patient and healthcare professional preferences and cost.[85] Surgery is often a major procedure that is followed by a structured rehabilitation program to prevent recurrence and dehiscence (wound separation).[9]
- For healable but refractory Stage 2 PU/PI, or for healable but refractory Stage 3/4 in the absence of surgical resources or if surgery is contraindicated, we suggest consideration for adjunctive therapies. See 'Adjunctive Therapies'.
- For non healable/ maintenance PU/PI: for elderly patients, with fatal illness or uncontrolled comorbidities, a palliative local wound care program is likely more appropriate.[7]
Types of surgical reconstruction
- Surgical closure of PU/PI can be achieved through direct closure, autologous skin graft, skin flap, composite flap, free tissue transfer or tissue expansion.[10][85] The current standard surgical method for closing PUs/PIs is to use composite flaps, preferably muscle or musculocutaneous flaps [7][10], or fasciocutaneous flaps if muscle function is needed (patients who can ambulate or transfer themselves) [86] Most common postoperative complications of PU/PI surgery include hematoma, seroma, infection and dehiscence. However, the most important complication is recurrence. Many patients/caregivers return to habits that originated the initial PU/PI.[86]
- For patients with stage 4 PU/PI and suspected osteomyelitis: Clinical guidelines recommend a combination of debridement, intravenous antibiotics and flap coverage.[6][7] To assist clinicians in decision making, the following surgical protocol may be helpful in managing acute and chronic osteomyelitis [10]:
-
- First, debride the ulcer bed and remove unhealthy granulation tissue over the underlying bone. Shave the surface of the bone (at a thickness of 5-6 mm) and send the specimen to histopathological examination.
- Second, assess viability of the exposed bone by checking bleeding, color and consistency. If bone is suspected to be non-viable (grayish, no bleeding, brittle bone), a sample of the deep bone should be sent for histopathological examination and bacteriological examination with culture and sensitivity.
- Once the remaining tissue is deemed viable, cover the ulcer with a muscle or musculocutaneous flap. Intravenous antibiotics are initiated, based on pre-operative soft tissue culture results, and administered for 5 days.
- If histopathological analysis of the deep bone specimen shows chronic osteomyelitis, antibiotics can be discontinued on the 5th day after surgery. If acute osteomyelitis is diagnosed, culture-guided antibiotics should be given for 6 weeks. If MRSA is detected, antibiotics are given for 8 weeks.[7]
Care before surgery
Prior to initiating any wound coverage procedure (i.e. skin autografts, flaps, or skin equivalents), it is recommended that:
- Patient condition and general health be optimized by ensuring adequate nourishment and glucose levels, and controlling comorbidities.[7] See section 'Nutrition' above
- Patient/caregiver are willing and able to adhere to perioperative care plan and plan to prevent recurrence.[6] Equipment for prevention/treatment should be procured before surgery (e.g., ideally, individual should be cared for on a high specification pressure mattress prior to surgery to test tolerance to the bed and confirm absence of problems such as dyspnea)[6]
-
The ulcer bed be prepared adequately, by removing slough, debris, necrotic tissue and management of bioburden levels, preferably to 10^5 CFU/g of tissue, with no beta hemolytic streptococci in the ulcer. A wound containing contaminated foci with greater than 10^5 CFU/g of tissue cannot be readily closed, as the incidence of wound infection that follows is 50–100%.[7]
- PU/PI is well-protected from urine and feces. [11] See section 'Excessive Moisture and Shear' above
- For patients with muscle spasms due to spinal cord injury or neurological disease, spasm management should begin at least 1 month before surgery.[10] Spasm can make it difficult to position the patient on the operating table and may predispose flap wound to dehiscence (separation of suture lines) and infection. Spasms can be medically managed with antispasmodic medication (e.g. baclofen, titrated up to a dose of 20-25 mg 4 times per day, and tapered down before complete discontinuation +/- diazepam 5mg 3 times a day).[10]
- If ulcer is in lower extremity, a reliable vascular status should be achieved: if the ulcer is granulating well after wound preparation, surgical coverage can be performed.[87] A well-granulating wound itself is an indication for good vascularity. However, if healing is stalling, then further evaluation using transcutaneous oxygen pressure measurement (TCOM) or angiograms may be warranted to evaluate the arterial flow and prepare for vascular intervention. See table with values and interpretations of non-invasive arterial tests in topic "How to Select Adequate Compression Therapy Pressure Levels and Products".
Care after surgery
- For patients who have undergone flap or skin graft reconstruction of a PU/PI, the NPUAP/EPUAP/PPPI guideline recommends use of a high specification support surface that provides enhanced pressure redistribution, shear reduction, and microclimate control.[6]
- The following protocol may be helpful [10]:
-
- Immediately following the surgery: most individuals can be transferred to an air fluidized bed (e.g. Clinitron). Patients at risk of aspiration, can be transferred to a bed with the top half made of air loss mattress and the lower half made of air fluidized bed (e.g. Rite Hite).
- In the forth week post flap surgery, paraplegic patients can be changed to an air loss mattress and initiate upper limb physical therapy. Tetraplegic patients can be kept on an air fluidized mattress until the sitting program is initiated.
- Sitting program is initiated at week 6 after flap surgery, provided no wound complications exist. Flaps may dehisce easily if subjected to excessive mechanical stress prior to the 6th week after surgery.
- As part of the discharge plan, patient and caregivers should receive education on how to prevent new or recurrent ulcers.[6] See topic "Pressure Ulcers/Injuries - Prevention"
Adjunctive Therapy
For healable PUs/PIs that do not show signs of improvement in 2-4 weeks of comprehensive care (i.e., refractory), adjunctive therapies to promote ulcer healing may be considered.[6][7][4] Comprehensive care includes treating the underlying causes, addressing patient's concerns and providing adequate local wound care. Evidence supporting adjunctive therapy interventions are not sufficiently strong to justify them as primary therapy. Choice of adjuvant therapy is based on clinical findings, availability of resources, and cost-effectiveness. Patient and ulcer should be re-evaluated prior to initiating adjunctive therapy. (See 'Plan Reassessment' above).
Adjunctive interventions with some evidence in promoting healing of refractory PUs/PIs include negative pressure wound therapy, electrical stimulation, ultraviolet C light, cellular and/or tissue products and autologous platelet-rich plasma. Coverage of adjunctive therapy by insurers is not uniform and it is advisable that insurance policies are checked prior to indication of these interventions.
Biophysical Interventions
Negative Pressure Wound Therapy (NPWT)
-
2CFor healable but refractory Stage 3 or 4 PUs/PIs without contraindications to negative pressure wound therapy (NPWT), clinicians might opt for NPWT as an adjunctive treatment to promote ulcer healing. (Grade 2C)
-
-
Rationale: Negative Pressure Wound Therapy, the application of continuous or intermittent negative pressure to wounds [10] may be used as an adjunctive therapy for deep, Stage 3 or 4 PU/PI [6][8], even before consideration for definitive flap coverage as long as ulcer is clean and there are no contraindications to NPWT. NPWT helps promote PU/PI healing through increased blood perfusion and granulation tissue, and decreased bacterial load.[7] Evidence of NPWT used in this context is considered of low certainty (evidence level C).[88][89] High cost of commercial NPWT products and access to trained personnel for application of NPWT dressings should be factored in when considering this treatment modality. NPWT is a Medicare-covered benefit for patients with PUs/PIs treated in the home and inpatient settings, provided requirements are met.[90] See section "Coding, Coverage and Reimbusement' in topic "Negative Pressure Wound Therapy"
- Contraindications: NPWT is contraindicated if patient cannot follow post NPWT application instructions, if the ulcer is inadequately debrided, necrotic, infected, malignant, has vital organs or vessels exposed, has no exudate, has a fistula, is actively bleeding.[6] Caution should be taken if the individual is on anticoagulant therapy.[6]
-
General instructions on how to select and apply NPWT devices can be found in the topic "How to Select and Apply Negative Pressure Wound Therapy Devices". For PU/PI patients, extra care should be taken during transfers and repositioning to keep the NPWT dressing well sealed and intact. If PU/PI is in the perineal area close to the anus, a bowel program or catheterization can help divert fecal material and urine.[7] Risks and benefits of a temporary colostomy should be discussed with the patient/caregivers.[10]
Electrical stimulation (ES)
-
2CFor healable but refractory stage 3 or 4 PU/PI, clinicians might opt for adjunct electrical stimulation (ES) to increase rate of wound healing, when resources are available and ES is covered by the patient's insurance. (Grade 2C)
-
-
Rationale: Electrical stimulation (ES) is the application of a small electrical charge through the wound, via electrodes placed on the periwound skin (examples include QuadStar Elite, BioMedical GV 350). ES may promote wound healing by replacing the current that naturally occurs in tissues, and is weak or absent in injured tissues. [91] ES parameters (e.g., voltage, continuous/pulsed current, etc) are typically not standardized across different care settings/institutions and treatment is usually customized to each patient.[91] In most protocols, ES is administered 5 to 7 times a week, once or twice daily, for 30 to 120 minutes.[91] Some clinical guidelines [6][7][8] suggest use of ES to treat healable, refractory Stage 2-4 PUs/PIs; however the NICE guideline recommends against its routine use, due to the low certainty evidence supporting its effectiveness in this context.[47] There is evidence that ES enhances healing of PU/PI in individuals with spinal cord injury.[92] ES may be especially beneficial as an adjunct for Stage 3 PU/PI treatment and to prevent flap breakdown after PU/PI surgical reconstruction. Two recent meta-analyses with RCTs at high or unclear risk of bias indicated that ES may be superior to standard wound care in promoting PU/PI healing (evidence level C).[91][93]
-
Coverage: Not all private insurers cover ES. Medicare covers ES performed for chronic wounds including stage 3 or 4 PU/PI that have not responded to standard wound care within 30 days, when indicated/performed by a physician or physical therapist (billable under HCPCS code G0281), and as long as signs of improvement are demonstrated within each 30 days of treatment.[94]
-
Contraindications: ES is contraindicated if patient has osteomyelitis, cancer, implanted electronic devices, lower extremity deep venous thrombosis, is pregnant, or while using wound dressings with metallic or ionic component.[91]
Pulsed Electromagnetic FIElDtherapy (EMT/PEMF)
-
2CWe suggest against pulsed electromagnetic field therapy (PEMF) as an adjunctive treatment of refractory PU/PI, until further evidence supporting its efficacy in this context becomes available (Grade 2C, against)
-
- Rationale: Electromagnetic therapy (EMT, also known as electromagnetic agent, electromagnetism, magnetic healing, magnetic field therapy) consists in the application of a field of electromagnetic energy that may be useful for wound healing. [95] Unlike other forms of electrotherapy, EMT does not use direct electrical effects or radiation (examples include Diapulse, PER 2000 HD). EMT may be delivered as pulsing current, known as pulsed electromagnetic field (PEMF). Most guidelines do not provide guidance on the use of EMT to treat PU/PI. The NPUAP/EPUAP/PPPIA guideline does not provide a positive or negative recommendation regarding EMT, but states that clinicians may consider PEMF treatment for recalcitrant Stage 2 PU/PI as well as any Stage 3 or 4 PUs/PIs.[6] However, it is still unclear if EMT is more effective than standard therapy in the treatment of PUs/PIs. A systematic review [95] with 2 RCTs at high or unclear risk of bias did not find statistically significant difference in complete PU/PI healing in people treated with EMT compared with those in the control group (evidence level C).
-
Coverage: Many U.S. private insurers do not cover EMT/PEMF to treat chronic wounds. Medicare covers PEMF performed for chronic wounds including stage 3 or 4 PU/PI that have not responded within 30 days of standard wound care, when indicated/performed by a physician or physical therapist (billable under HCPCS code G0329), and as long as signs of improvement are demonstrated within each 30 days of treatment. [94]
-
Contraindications: PEMF is contraindicated in individuals with pacemakers or other electrical implants, pregnancy or organ transplant, and should be used with caution if fever, active bleeding, seizures or dehydration.[6]
DIATHERMY
- Short wave diathermy is the non-contact application of a continuous magnetic field that produces significant heating of tissue 3-5 cm below surface without overheating skin. It causes vasodilation and increased blood flow and has been used to decrease inflammation, edema, lymphedema and pain. Clinical guidelines do not provide guidance on use of diathermy to treat PU/PI. No RCTs on use of diathermy to treat PU/PI has been identified.
-
Coverage: Diathermy (CPT code 97024) to treat wounds is not covered by many U.S. private insurers. Each Medicare Administrative Contractor (MAC) determines if diathermy is considered medically necessary. Some MACs listed on their local coverage determinations (LCDs) that diathermy is medically necessary for the delivery of heat to deep tissues such as skeletal muscle and joints for the reduction of pain, joint stiffness, and muscle spasms.[96][97]
- Contraindications: diathermy is not indicated for patients with malignancy, sensory loss, metallic implants or foreign bodies, pregnancy, active menses, application over moist dressing, ischemic areas or arteriosclerosis, thromboangiitis obliterans, phlebitis, cardiac pacemarkers.
Therapeutic UltRASOUND
-
2CFor healable but refractory PU/PI, we suggest against routine use of non-contact low frequency ultrasound spray (NC-LFUS) as an adjunctive therapy, due to insufficient evidence supporting its use for PU/PI. (Grade 2C, against)
-
-
Rationale: Non-contact low-frequency ultrasound spray (NC-LFUS) is meant to simultaneously debride and cleanse wounds. The device has a disposable handset that is held ~1cm away from the wound and sprays saline solution, generating mist and ultrasonic energy at 40 kHz. Ultrasonic energy at this level supposedly stimulates angiogenesis, growth factor production. (example: Mist Therapy System). Most clinical guidelines do not provide guidance on the use of HFUS to treat PU/PI. The NPUAP/EPUAP/PPPIA guideline does not provide a positive or negative recommendation regarding NC-LFUS, but states that NC-LFUS is not recommended for routine use at this time due to insufficient evidence to support or refute its use in this context.[6] No RCTs evaluating the effectiveness on NC-LFUS in treating PU/PI specifically have been identified. Many case reports and retrospective studies on the use of NC-LFUS are available, however the design of these types of studies results in evidence with lower level of certainty as compared to that generated by RCTs.[12][13][98] Studies evaluating NC-LFUS on other types of ulcers [99] are not immediately applicable to PU/PI, due to the different etiology and different treatments effectiveness.
-
Coverage: Medicare covers NC-LFUS (specifically, Mist Therapy, CPT code 97610) to treat chronic ulcers, provided requirements are met, however most private insurers do not offer coverage for NC-LFUS as an adjunct to treatment of chronic ulcers. Cost of the device and disposable handset may be significant and should be factored in as well. See topic "Other Biophysical Agents".
-
Contraindications: NC-LFUS should not be used near prostheses, near electronic implanted devices (e.g., cardiac pacemakers), over the lower back or uterus in pregnant women; over areas of malignancy; or on the face/head.[6] Caution should be taken by healthcare providers during application - the tip of the handset may cause shock and burns when touched.[100]
-
2CFor healable but refractory PU/PI, we suggest against routine use of direct contact high-frequency ultrasound (HFUS) as an adjunctive therapy, due to current conflicting evidence supporting its use and uncertain coverage by insurers. (Grade 2C, against)
-
-
Rationale: Direct contact high-frequency ultrasound (HFUS) is the application of high-frequency, thermal ultrasound waves (in the range of MHz) to the ulcer and periwound (examples include Intelect Adanced, SoLo Therasonic 355). HFUS may stimulate activity of cells important for wound healing (e.g., macrophages, fibroblasts), collagen and growth factor secretion.[101] Most clinical guidelines do not provide guidance on the use of HFUS to treat PU/PI. The NPUAP/EPUAP/PPPIA guideline does not provide a positive or negative recommendation regarding HFUS, but states that clinicians might consider HFUS as an adjunct for the treatment of infected PU/PI.[6] However, evidence supporting use of HFUS as an adjunctive therapy to treat non-healing PU/PI is conflicting and of low certainty (evidence level C). Meta-analysis of 2 RCTs showed no difference in PU/PI healing between groups treated with HFUS and groups treated with standard wound care alone.[102] On the other hand, a more recent RCT found that the proportion of PUs/PIs that healed in 6 weeks of treatment with HFUS was significantly higher than the proportion that healed with standard wound care alone.[101] Medicare and most private insurers do not cover HFUS for treatment of PU/PI. See section 'Coding, Coverage and Reimbursement' in "Biophysical Agents (Other)".
Phototherapy
-
2CFor refractory but healable PU/PI, clinical guideline suggests against routine use of infrared therapy or laser therapy as an adjunctive treatment to promote would healing, due to insufficient evidence supporting its use and lack of coverage by insurers. (Grade 2C, against)
-
2CFor refractory but healable stage 2 - 4 PU/PI, clinicians might opt to consider short term application of ultraviolet C light (UVC) as an adjunctive treatment to promote wound healing, if other therapies fail and if covered by insurance. (Grade 2C)
-
-
Rationale: Phototherapy includes use of light (infrared, laser, ultraviolet) to treat some cutaneous conditions. Ultraviolet C light has bactericidal properties and may be helpful in controlling bioburden when conventional methods have failed.[103] Most clinical guidelines do not provide guidance on the use of phototherapy to treat PU/PI. The NPUAP/EPUAP/PPPIA guideline does not provide a positive or negative recommendation regarding phototherapy, but states that infrared and laser therapy are not recommended as an adjuncts for the treatment of PU/PI at this time due to insufficient evidence to support or refute its use in this context. It also states that clinicians might consider short term application of ultraviolet C light (UVC) if other therapies fail.[6] There is low certainty evidence supporting use of ultraviolet therapy and low-level laser therapy as adjuncts to treat PU/PI, however studies are at risk of bias and sample sizes of the studies were small and results might have occurred by chance.
-
Coverage: Ultraviolet therapy (CPT code 97028) is not covered by many U.S. private insurers for treatment of PU/PI. Each Medicare Administrative Contractor (MAC) determines if ultraviolet is considered medically necessary. Some MACs mention on their local coverage determinations (LCDs) that ultraviolet therapy is medically necessary for the patient requiring the application of a drying heat (i.e. a patient having an open wound and severe psoriasis limiting range of motion). [96][97]
HYPERBARIC OXYGEN THERAPY (HBO)
- 1CWe recommend against use of hyperbaric oxygen therapy (HBOT) as an adjunctive therapy for non-healing PUs/PIs without any other indication for HBOT (Grade 1C, against)
-
- Rationale: Clinical guidelines [6][7][47] recommend against use of HBOT to treat PUs/PIs due to lack of sufficient evidence. To date, no RCTs evaluating HBOT as a treatment of PU/PI has been identified. Use of HBOT to treat PU/PI is not covered by Medicare, but HBOT may be covered for a patient with PU/PI if it is medically necessary for the treatment of another condition.[104] See HBOT indications in topic "An Introduction to Hyperbaric Oxygen Therapy"
Wound Coverage
CELLULAR AND/OR TISSUE PRODUCTS (CTPS)
- 2CFor healable but refractory Stage 3 or 4 PUs/PIs that are fully granulated, but still have a significant non-epithelialized area and no exposed vessels/bone, cellular and/or tissue products (CTPs) may be used in lieu of skin grafting, to promote wound healing, if CTP is covered by the patient's insurance.[11] (Grade 2C)
-
-
Rationale: Most clinical guidelines do not provide guidance on use of cellular and/or tissue products (CTPs), also known as "skin substitutes", to treat PU/PI. The 2014 NPUAP/EPUAP/PPPIA guideline, suggests against routine use of CTP to treat PUs/PIs due to lack of sufficient evidence to support or refute its use in the treatment of PUs/PIs at the time the guideline was published.[6] Evidence of use of CTPs for PUs/PIs as reported by RCTs is relatively scarce. Many case reports and retrospective studies are available, however the design of these types of studies results in evidence with lower level of certainty as compared to that generated by RCTs. We have identified a few RCTs (all published after the NPUAP/EPUAP/PPPIA guideline), and summarized in the section 'Pressure Ulcers/Injuries' in "Cellular and/or Tissue Products". There is some evidence that suggests that amniotic membranes [105], ORC/collagen matrix [106] and extracellular wound matrix made from porcine small intestinal submucosa [107] may be more effective than standard care in promoting PU/PI healing. However, data are derived from a few RCTs and more trials are needed before specific recommendations can be made.
-
Coverage: Not all Medicare Administrative Contractors (MAC) cover CTPs for refractory PUs/PIs. It is recommended that clinicians check their MAC's local coverage determination for specific details.
Other biologics
AUTOLOGOUS PLATELET-RICH PLASMA (PRP)
-
2CFor non-infected, healable but refractory Stage 3 or 4 PUs/PIs, autologous Platelet-Rich-Plasma (PRP) may be considered as an adjunctive therapy to treat refractory PUs/PIs, when other interventions have been tried and failed.(Grade 2C) Note: this intervention is typically not covered by Medicare
-
-
Rationale: Some clinical guidelines suggest clinicians consider use of autologous Platelet-Rich-Plasma (PRP) as adjunctive therapy for Stage 3 or 4 PUs/PIs.[6][8][7] However, evidence supporting use of PRP to treat refractory PU/PI is of low certainty. A 2016 systematic review found that it is currently unclear whether adjunctive PRP is better than standard of care alone in promoting healing of chronic wounds in general.[108] RCTs that focus on PRP specifically for PUs/PIs are scarce. However, we identified one small RCT[109] that showed a significantly higher proportion of PUs/PIs that completely healed at 36 days in the groups that received PRP or PRP plus hyaluronic acid (HA), compared to standard of care alone.(evidence level C) When considering use of PRP as an adjunctive therapy, it is important to bear in mind that use of these interventions require trained personnel, can be costly, and are not covered by Medicare or other private insurance plans (except when part registered clinical trials).[110] Some PRP medical devices (e.g, 3C Patch® System, Autologel) have received FDA clearance for treatment of PUs/PIs.
PLATELET-DERIVED GROWTH FACTOR (PDGF)
-
2CFor patients with healable but refractory PUs/PIs, we suggest against use of recombinant human platelet-derived growth factor (becaplermin) to promote ulcer healing (Grade 2C, against)
-
-
Rationale: Growth factors are important for normal healing, and usually deficient in chronic wounds.[7] Some clinical guidelines [6][8] suggest consideration of PDGF as an adjunct therapy for refractory PUs/PIs, and it may be a cost-effective treatment for Stage 3 and 4 PUs/PIs. [111] However, evidence supporting its use as an adjunctive therapy for non-healing PU/PI is conflicting.[7][112][113][114] Becaplermin (Regranex) has been used as an adjunctive treatment for refractory DFUs but the FDA has not yet approved its use on PUs/PIs.[114]
APPENDIX
Summary of Evidence
Pressure Redistribution
(back to text)
Clinical guidelines
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (NPUAP/EPUAP/PPPI), Wound Healing Society (WHS), Wound, Ostomy and Continence Nurses (WOCN) Society [7][6][8]
| Intervention |
NPUAP/EPUAP/PPPI
|
WHS |
WOCN |
utilization of support surfaces that meet the individual's needs and are compatible with the care setting to promote PU/PI healing.
|
Strong C |
Level I |
Class I C |
Meta-analyses
- A 2018 network meta-analysis found that compared with standard hospital surfaces, there is moderate-certainty evidence that powered active air surfaces and powered hybrid air surfaces probably reduce pressure ulcer incidence compared with standard hospital surfaces (risk ratios (RR) 0.42, 95% confidence intervals (CI) 0.29 to 0.63; 0.22, 0.07 to 0.66, respectively).[16]
- A 2018 meta-analysis with 19 RCTs (3241 participants) analyzed effectiveness of based on the current evidence, it is unclear whether any particular type of low- or high-tech support surface is more effective at healing pressure ulcers than standard support surfaces. [19]
SOE-Re(Positioning)
(back to text)
Clinical guidelines
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (NPUAP/EPUAP/PPPI), Wound Healing Society (WHS), Wound, Ostomy and Continence Nurses (WOCN) Society [7][6][8]
| Intervention |
NPUAP/EPUAP/PPPI
|
WHS |
WOCN |
Reposition all individuals at risk of, or with existing pressure ulcers, unless contra-indicated
|
Strong A |
Level II |
Class I C |
Meta-analyses
-
A 2015 Cochrane systematic review found no randomized controlled trial (RCT) evidence that addresses the question of whether repositioning patients improves the healing rates of PU/PI. Authors concluded that despite the absence of RCTs, it is reasonable to suggest that individuals with PU/PI be repositioned to avoid depriving the wounded area of oxygen and nutrients which are needed for tissue repair.[31]
Randomized clinical trials (RCT)
- No RCTs that address the question of whether repositioning patients improves the healing rates of PU/PI have been identified
SOE - Nutrition
(back to text)
Systematic reviews
- A 2017 systematic review included 7 RCTs with 369 patients; all RCTs reported that arginine-enriched enteral nutrition led to a significant improved PU/PI healing compared with standard hospital diet in 2-12 weeks follow-up. Authors concluded that arginine-enriched enteral nutrition led to a significant improvement in PU healing. It was effective not only in malnourished patients, but also in non-malnourished patients. [42]
- A 2017 systematic review and meta-analysis included 3 RCTs. Compared with control interventions, formulas enriched with arginine, zinc and antioxidants resulted in significantly higher reduction in ulcer area (-15.7% [95%CI, -29.9, -1.5]; P=0.030; I2=58.6%) and a higher proportion of participants having a 40% or greater reduction in PU size (OR=1.72 [95%CI, 1.04, 2.84]; P=0.033; I2=0.0%) at 8 weeks. A nearly significant difference in complete healing at 8 weeks (OR=1.72 [95%CI, 0.86, 3.45]; P=0.127; I2=0.0%) and the percentage of change in the area at 4 weeks (-7.1% [95%CI, -17.4, 3.3]; P=0.180; I2=0.0%) was also observed. Authors concluded that the use of formulas enriched with arginine, zinc and antioxidants as oral supplements and tube feeds for at least 8 weeks are associated with improved PU healing compared with standard formulas. [40]
SOE - Cleansing
(back to text)
Clinical guidelines
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (NPUAP/EPUAP/PPPI), Wound Healing Society (WHS), Wound, Ostomy and Continence Nurses (WOCN) Society [7][6][8]
| Intervention |
WOCN |
NPUAP/EPUAP/PPPI
|
WHS |
Cleanse the wound with potable tap water, distilled water, cooled boiled water, or saline/salt water.
|
Class IB |
Weak C |
Level III |
Consider use of antiseptics for "maintenance wounds," which are defined as wounds that are not expected to heal, or for wounds that are critically colonized.
|
Class IC |
Weak C |
Level III |
Systematic reviews:
- A 2013 systematic review [66] included 3 RCTs (169 participants) comparing the effect of cleansers for treating PUs/PIs. No studies compared cleansing with no cleansing. No statistically significant difference in healing was observed when water and saline were compared. A statistically significant difference favoring the intervention was found when saline spray containing Aloe vera, silver chloride and decyl glucoside (Vulnopur) was compared with isotonic saline (P value = 0.025), and when pulsatile lavage was compared with sham (the lavage flow was directed into a wash basin positioned adjacent to the wound and not visible to the participants) (MD -6.60, 95% CI-11.23, -1.97). Studies were considered of low certainty evidence due to biases (small sample size, selection bias, allocation bias). Authors concluded that there is no evidence strong enough to recommend one cleansing solution/pressure over another.
SOE - Debridement
(back to text)
Clinical Guidelines
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (NPUAP/EPUAP/PPPI), Wound Healing Society (WHS), Wound, Ostomy and Continence Nurses (WOCN) Society,National Institute for Health and Care Excellence (NICE), [7][8][47][6]
| Intervention |
NPUAP/EPUAP/PPPI
|
WHS |
WOCN |
NICE |
Debride devitalized tissue within the wound bed or edge of PU/PI to promote healing, when consistent with the patient's condition and goals of therapy
|
Strong C
|
Level I
|
Class I C
|
In favor (no grading)
|
Systematic reviews
- no systematic reviews on debridement to treat PU/PI were identified
SOE -Moisture management and dressing selection
(back to text)
Sytematic reviews and meta-analyses
- A 2017 network meta-analysis [82] including 39 RCTs observed that none of the interventions with moderate or low-quality evidence appears to result in a higher proportion of PU/PI healed. Many trials are small and at high risk of bias. It is not clear whether regimens involving protease-modulating dressings increase the probability of pressure ulcer healing compared with saline gauze (risk ratio (RR) 1.65, 95% confidence interval (CI) 0.92 to 2.94) (moderate-certainty evidence). It is unclear whether these interventions increase the probability of healing compared with saline gauze (low-certainty evidence): collagenase ointment (RR 2.12, 95% CI 1.06 to 4.22); foam dressings (RR 1.52, 95% CI 1.03 to 2.26); basic wound contact dressings (RR 1.30, 95% CI 0.65 to 2.58) and polyvinylpyrrolidone plus zinc oxide (RR 1.31, 95% CI 0.37 to 4.62). Authors concluded that there is currently insufficient evidence to judge whether any one dressing or topical treatment increases the probability of pressure ulcer healing compared with others (and neither is there sufficient evidence to judge whether there is a negative relative impact on wound healing or no relative impact).
SOE - Negative Pressure Wound Ther apy
(back to text)
Clinical guidelines
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (NPUAP/EPUAP/PPPI), Wound Healing Society (WHS), Wound, Ostomy and Continence Nurses (WOCN) Society,National Institute for Health and Care Excellence (NICE), [7][8][47][6]
| Intervention |
NPUAP/EPUAP/PPPI
|
WOCN |
WHS |
NICE |
| Use of NPWT as an adjuvant for treatment of Stage 3 or 4 PU/PI |
Weak, B |
Class I B |
Level I |
Do not routinely use NPWT for PU/PI (no grading) |
Systematic review/ meta-analysis
- A 2015 Cochrane systematic review[89] included 4 RCTs (149 participants) and concluded that there is low certainty about the potential benefits or harms, or both, of using negative pressure wound therapy (NPWT) for PU/PI management. Meta-analysis was not conducted due to to the heterogeneity of the RCTs' designs and outcomes. Two studies compared NPWT with dressings; one study compared NPWT with a series of gel treatments and one study compared NPWT with 'moist wound healing'. One study had a 24-week follow-up period, and two had a six-week follow-up period, the follow-up time was unclear for one study. Overall there is low quality and inconclusive evidence regarding the clinical effectiveness of NPWT as a treatment for pressure ulcers. Authors suggested that given the current uncertainties, when choosing between alternative treatment options for pressure ulcers, practitioners may elect to consider characteristics such as costs and symptom management properties.
Randomized controlled trials (RCT)
-
One new RCT after publication of the Cochrane systematic review was identified: A 2016 small RCT (60 participants) [88] compared the effect of a self-assembled NPWT device on the healing of Stage 3 or 4 PUs/PIs with standard care. Length and width were significantly (p<0.01) decreased in the NPWT group as compared with the standard care group at week 9. This RCT can be considered of low or unclear certainty (evidence level C) due to use of a surrogate endpoint, lack of blinding of assessors, patients and healthcare personnel, and small sample size.
SOE - Electrical stimulation
(back to text)
Clinical guidelines
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (NPUAP/EPUAP/PPPI), Wound Healing Society (WHS), Wound, Ostomy and Continence Nurses (WOCN) Society,National Institute for Health and Care Excellence (NICE), [7][8][47][6]
| Intervention |
NPUAP/EPUAP/PPPI
|
WHS |
WOCN |
NICE |
| Electrical stimulation to treat refractory PU/PI |
Weak, A |
Level I |
Class I A |
Do not use routinely (no grading) |
Systematic reviews/meta-analyses
-
A 2018 systematic review included 9 RCTs and 2 case series studies.[93] As for included RCTs, there was some overlap with the ones included in the Ontario Health Technology Assessment.[91] 5 RCTs were included in the meta-analysis. Authors concluded that high-voltage monophasic pulsed current (HVMPC) plus standard wound care were more effective than standard wound care with or without sham HVMPC in reducing stage 2-4 PU/PI areas. Also, the cathodal HVMPC protocol was found to be superior to the cathodal-anodal HVMPC protocol.[115] However, studies utilized surrogate endpoints (only evaluated rate of healing and not how many ulcers healed), and were not blinded. Many were of small size. Evidence can be thus be considered of low certainty (level C).
- A 2017 Ontario Health Technology Assessment included 9 RCTs and 2 non-RCTs. [91] Authors concluded that while electrical stimulation is a safe intervention (GRADE quality of evidence: high certainty, A), it is unclear whether it improves wound healing (GRADE quality of evidence: low certainty, C). There was no significant difference in complete PU/PI healing between adjunct electrical stimulation and standard wound care (6 RCTs). There was a significant difference in wound area reduction favoring electrical stimulation compared with standard wound care (meta-analysis of 6 RCTs). However, area reduction is a surrogate endpoint and does not provide direct evidence of healing. As for cost-effectiveness, no studies were found.
Randomized controlled trials (RCTs)
- no new RCTs published since publication of the 2018 systematic review have been identified
SOE - Pulsed electromagnetic therapy
(back to text)
Clinical guidelines
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (NPUAP/EPUAP/PPPI), Wound Healing Society (WHS), Wound, Ostomy and Continence Nurses (WOCN) Society, National Institute for Health and Care Excellence (NICE), [7][8][47]
| Intervention |
NPUAP/EPUAP/PPPI
|
WHS |
WOCN |
NICE |
| Pulsed electromagnetic therapy to treat refractory PU/PI |
No specific recommendation icon, C. But text says "Consider the use of pulsed..."
|
not mentioned |
not mentioned |
not mentioned
|
Systematic review
- A 2015 Cochrane systematic review included 2 RCTs (60 participants).[95] Authors concluded that it is unclear if electromagnetic therapy (EMT) is more effective than standard therapy with sham therapy in the treatment of PUs/PIs. None of the studies found a statistically significant difference in complete healing in people treated with EMT compared with those in the control group. In one trial that assessed percentage reduction in wound surface area, the difference between the two groups was reported to be statistically significant in favor of EMT (RR 37%, 95% CI 17.36 to 56.64), however this result needs to be interpreted with caution, as the evidence generated by the RCT is of low certainty (due to small sample size, and unclear randomization sequence, concealment allocation and blinding of outcome assessor). Both RCTs were small and findings could be due to chance. Also, percentage reduction in ulcer area is a surrogate endpoint, which is less clinically relevant than complete healing. The other trial did not assess healing rate, just complete healing. (Evidence level C).
Randomized controlled trials (RCTs)
- No new RCTs published since publication of the 2015 systematic review have been identified
SOE - Therapeutic Ultrasound
(back to text)
Clinical guidelines
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (NPUAP/EPUAP/PPPI), Wound Healing Society (WHS), Wound, Ostomy and Continence Nurses (WOCN) Society,National Institute for Health and Care Excellence (NICE), [7][8][47][6]
| Intervention |
NPUAP/EPUAP/PPPI
|
WHS |
WOCN |
NICE |
| Noncontact low frequency (40 kHz) ultrasound spray (NC-LFUS) to treat refractory PU/PI |
No specific recommendation icon, C. But text says "NC-LFUS is not recommended for routine use at this time" |
not mentioned |
not mentioned |
not mentioned
|
Contact low frequency (22.5, 25 or 35 kHz) ultrasound for debridement of necrotic soft tissue (not eschar)
|
No specific recommendation icon, C. But text says "Consider use of low frequency..."
|
not mentioned |
not mentioned |
not mentioned |
Contact high frequency (MHz) thermal ultrasound as an adjunct for the treatment of infected pressure ulcers
|
No specific recommendation icon, C. But text says "Consider use of high frequency..."
|
not mentioned |
not mentioned |
not mentioned |
Non-contact low frequency ultrasound spray (NC-LFUS)
Systematic review
- no systematic reviews focusing on NC-LFUS to specifically treat PU/PI have been found. There are systematic reviews covering chronic wounds as a collective, however evidence provided is not directly applicable to PU/PI. Chronic ulcers have different etiologies and different treatment effectiveness.
Randomized controlled trials (RCTs
- no RCTs focusing on NC-LFUS to treat PU/PI specifically have been found
High frequency ultrasound
Systematic review
- A 2006 Cochrane systematic review [102] included 3 RCTs (146 participants) that evaluated therapeutic high-frequency ultrasound (~3Mhz) on the healing of non-infected PUs/PIs. Two RCTs compared ultrasound therapy with sham ultrasound and the third compared a combination of ultrasound and ultraviolet light with laser and with standard treatment. None of the 2 RCTs comparing ultrasound with sham found significant difference in healing rates. In a pooled analysis with the first 2 RCTs (128 participants), there was no evidence of benefit associated with the use of ultrasound in the treatment of pressure ulcers (95% CI 0.65 to 1.45). Authors concluded that there is no evidence of a benefit of using ultrasound therapy in the treatment of pressure ulcers. The possibility of a beneficial or a harmful effect cannot be ruled out due to the very small number of trials.
Randomized controlled trials (RCTs)
- A 2016 RCT [101] (77 participants with Stage 2-4 PU/PI) compared standard wound care (SWC), SWC+Ultrasound - US (1MHz; 0.5 W/cm 2 ; 20%; 1–3 minutes/cm 2 ); or SWC+Electrical Stimulation - ES (HVMPC, 154 µs, 100 pps, 100 V, 250 µC/sec, 50 minutes/day). US and ES were administered once a day, 5 days a week. The percentage reduction in the surface area of PUs at 6 weeks was significantly greater in the SWC+US group (p=0.024) and the SWC+ES group (p=0.030) versus the control group. The SWC+ES group also had a significantly greater proportion of PUs that decreased in area by at least 50% or closed than the control group (p=0.05 and 0.031, respectively). No difference was found between WC+US and SWC+ES groups. At week 6, 15 of 29 (51.72 %) PUs in the ES group completely closed, versus seven of 31 PUs (22.58 %) in the control group (p=0.031). In the US group, 13 of 28 PUs (46.43 %) closed - more than in the control group, but not statistically significant (p=0.097). Authors concluded that HFUS and HVMPC are comparable regarding their effectiveness in reducing the size of PUs in older people. Of note, only the US group achieved statistically significant higher proportion of ulcers closed. Evidence can be considered of low certainty (evidence level C) due to small sample size, lack of patient blinding.
- A 2014 RCT [116] (42 participants) compared standard wound care (SWC) with or without high frequency ultrasound (HFUS, 1 MHz, 0.5 W/ cm2, duty cycle of 20%, 1-3 minutes/cm2; one session per day, 5 days a week). The percentage reduction in the surface area of PU/PIs at 6 weeks was significantly higher than in the SWC group P = 0.047). Percentage of ulcers closed was not statistically different between the two groups. Evidence can be considered of low certainty (evidence level C) due to small sample size, lack of patient blinding.
SOE - Phototherapy
(back to text)
Systematic reviews
- A 2017 systematic review [117] included 4 RCTs that studied application of low-level laser therapy (LLT) in the treatment of PUs/PIs. One study compared to different single wavelengths showed a significant 71% reduction of the PU and an improved healing rate in which 47% of PU healed completely after 1 month of therapy with the use of LLT with a wavelength of 658 nm. The other analyzed wavelengths were not significant in the assessed outcomes. All studies were considered at high/ unclear risk of bias (evidence level C).
- A 2014 Cochrane systematic review [118] included 7 RCTs (403 participants), and concluded that it is unclear if phototherapy is effective in treating PUs/PIs. 6 RCTs compared the use of phototherapy with standard care only; one trial compared it with standard care plus sham phototherapy. As for ultraviolet (UV): 2 RCTs showed the ultraviolet (UV) treated group had a shorter mean time to complete healing than the control group (mean difference -2.13 weeks (95% CI -3.53 to -0.72, P value 0.003)). As for laser: 1 RCT reported that the laser group had a longer mean time to complete healing than the control group (mean difference 5.77 weeks; 95% CI -0.25 to 11.79). Among five studies reporting the rate of change in ulcer area, three studies found no statistically significant difference between the two groups. The results were based on data from trials with unclear risk of bias for which generation of the randomization sequence, concealment allocation and blinding of outcome assessors were unclear. The quality of evidence is very low due to the unclear risk of bias and small number of trials available for analysis.
Randomized controlled trials (RCTs)
- no new RCTs published after publication of the 2015 systematic review have been identified
SOE - Other Bio logics
(back to text)
Clinical guidelines
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (NPUAP/EPUAP/PPPI), Wound Healing Society (WHS), Wound, Ostomy and Continence Nurses (WOCN) Society [7][8][6]
Different recommendation strength and levels of evidence, possibly due to different evidence assessment methods.
| Intervention |
NPUAP/EPUAP/PPPI
|
WOCN |
WHS |
| Use platelet-derived growth factors (e.g. becaplermin) to treat refractory PU/PI |
Weak C |
Class IB |
- |
| Use platelet-rich plasma to treat refractory PU/PI |
- |
- |
Level II |
Platelet-rich plasma
Systematic review/ meta-analyses:
- A 2016 systematic review with 8 RCTs (391 participants) evaluated if platelet-rich plasma (PRP) improves healing of chronic wounds compared with standard treatment, and found that it is currently unclear if PRP is better than standard care (risk ratio (RR) 1.19, 95% confidence interval (CI) 0.95 to 1.50; I2 = 27%). Included trials were of low certainty (trials are small/underpowered to detect treatment effects, if they exist, and are generally at high or unclear risk of bias). PUs/PIs were not separately analyzed.[108]
Randomized Controlled Trials (RCTs):
- One RCT specific to PU/PI has been identified: A 2014 RCT compared use of platelet-rich growth factor (i.e. platelet-rich plasma activated with 10.0% calcium chloride, PRGF), PRGF plus hyaluronic acid (HA) and standard care in the healing of refractory Stage 2-3 PUs/PIs. Results assessed at the 36th day, showed that a significant reduction in ulcer area(p=.001) was observed in all intervention groups, with a mean area reduction of more than 48.0% versus baseline. The greatest mean reduction (80.4% vs. baseline, p =.004) was seen in the group treated with 2 doses of PRGF plus HA. Complete wound healing was observed in 32.0% of PUs treated with two doses of PRGF (p=.002) and in 37.5% of those treated with two doses of PRGF plus HA (p =.004). Upon GRADE assessment, evidence is considered of level C, due to small sample size of the individual groups, significant differences in patient baseline parameters across groups (e.g., ulcer location and stages), unclear blinding of healthcare professionals, assessors and patients.[109]
Platelet-derived growth factor (i.e becaplermin)
Systematic review
Randomized Controlled Trials (RCTs):
-
A 1994 small RCT (41 patients) [113] compared efficacy of the daily topical application of recombinant platelet-derived growth factor-BB (rPDGF-BB) with standard care in the treatment of PU/PI. When adjusted for initial volume, ulcer volume after 28 days of treatment was smaller in the rPDGF-BB-treated groups compared with the placebo group (analysis of covariance, P = .056). Results of this small trial were not statistically significant though, so it is unclear whether PDGF is more effective than standard care in promoting healing of PU/PI.
- A 1999 industry-sponsored RCT (124 participants) [112] found that once-daily treatment of chronic Stage 3 or 4 PUs/PIs with becaplermin gel 100 microg/g or 300 microg/g significantly increased the incidences of complete and >/= 90% healing and significantly reduced the median relative ulcer volume at endpoint compared with that of placebo gel (p < 0.025 for all comparisons). However, groups within the trial were of small size, increasing the risk for imprecision. Also, it is unclear if patients were lost to follow up.
-
A 2018 cost-effectiveness analysis utilizing data from the RCT above found that expected annual direct costs for PU/PI were $3827 for the becaplermin group and $1279 for the control group. The incremental cost-effectiveness ratio was $298 (about $43/day), indicating that patients would have to pay an extra $298 to gain 1 additional PI-free week. Authors concluded that becaplermin yielded better outcomes at a slightly higher cost than standard care. [111]