INTRODUCTION
Treatment Protocol Guidelines
The following hyperbaric medicine treatment protocol is based upon the recommendations of the Hyperbaric Oxygen Committee of the Undersea and Hyperbaric Medical Society.[1] Clinical protocols and/or practice guidelines are systematically developed statements that help physicians, other practitioners, case managers and clients make decisions about appropriate health care for specific clinical circumstances.
Protocols allow health providers to offer evidence-based, appropriate, standardized diagnostic treatment and care services to patients undergoing hyperbaric oxygen therapy (HBOT). This section discusses Soft Tissue Radiation Necrosis (STRN). Evidence-based medicine offers clinicians a way to achieve improved quality, improved patient satisfaction, and reduced costs. Utilization Review should be initiated when clinical decisions result in deviation from or modification of treatment protocols. This includes any course of treatment at or above the recognized threshold limits.
Medical Necessity
Medicare.gov defines “medically necessary” as “health-care services or supplies needed to prevent, diagnose, or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.”
The following condition meets coverage indications per the National Coverage Determination (NCD) 20.29.[2] Continued HBOT without documented evidence of effectiveness does not meet the Medicare definition of medically necessary treatment. Thorough re-evaluation should be made at least every 30 days for documentation of response to therapy.
TREATMENT PROTOCOL
(SKIN, PELVIC, BLADDER, RECTUM, COLON, CNS, LARYNX, BONY NECROSIS)
| Background | Delayed (also known as 'late' or 'chronic') effects of radiation are a complication of modern radiotherapy, which can be treated with HBOT. Note that these chronic effects are to normal tissues that are juxtaposed to tumor tissue. This is often referred to in radiation oncology as LENT (Late Effects to Normal Tissues) Some examples of delayed radiation effects include soft tissue radionecrosis (Figures 1-3), radiation cystitis, radiation proctitis (Figure 4), and laryngeal chondroradionecrosis. The basic pathophysiology of delayed radiation tissue damage is an obliterative endarteritis with resultant tissue hypoxia and secondary fibrosis. |
| Goals of HBOT |
- Reduce tissue fibrosis and breakdown by inducing neovascularization in the radiated tissue and improving tissue oxygenation
- Prevent wound dehiscence following soft tissue reconstructive surgery in previously irradiated areas
|
|
Diagnosis
|
- Delayed radiation complications often manifest as non-healing wounds in previously irradiated areas. The wounds can be precipitated by an external insult such as surgery, trauma, even minor trauma. Some of these wounds are visible and some are not (e.g., radiation cystitis, vaginitis, proctitis, and urethritis).
- It is important to differentiate delayed radiation injuries from acute radiation injuries, which usually resolve within a few weeks to a few months from radiation exposure and are treated symptomatically (e.g., radiation dermatitis and/or skin burns).
|
|
Hyperbaric Criteria
|
- Non-healing wound within a previously irradiated area with at least six months since last radiation exposure
- History of radiation treatment (usually in excess of 40 Gray or 4,000 cGy, although the dose may vary according to the tissue type and malignancy) to the region of the documented injury.[3][4][5]
- Wound that is non-responsive to conservative standard treatment
|
|
Evaluation
|
- Comprehensive history, to include:
- Date cancer diagnosed
- Date radionecrosis diagnosed
- Type of radiation source (e.g., electron beam is much less harmful than neutron beam). Total dose over total number of treatments. Radiation fraction administered (e.g., "Thirty treatments of electron beam radiation to the prostate gland in 200 cGy fractions for a total of 6,000 cGy. The prostatic urethra remained in field and has been affected."
- Radiation date span
- Previous treatment or therapies
- Obtain the radiation-oncology reports
- Physical examination (Try to identify the radiation port tattoos, if possible.)
- Labs to order or review:
- Complete Blood Count (CBC)
- Serum Albumin
- Pre-albumin
- Erythrocyte Sedimentation Rate (ESR)
- C-reactive protein (CRP)
- Wound photographs (if possible)
- Chest x-ray (provider discretion)
- Electrocardiogram (ECG) (provider discretion)
- Determine present oncological status (e.g., remission, local recurrence, metastasis, etc.)
- Evaluation of tympanic membranes pre- and post-treatment as needed
- Baseline visual acuity assessment
- Smoking/nicotine cessation
- Nutritional screening
|
|
Treatment
|
HBOT treatment protocol for cystitis or proctitis
- 2.0-2.5 ATA (Be Specific) oxygen for 90-120 minutes of oxygen breathing (Table 1 or 3)
- Once daily basis for 40 treatments
- Referring physician examines the area under direct visualization after 40 treatments and together with the HBO physician decides if to continue to 60 treatments.[6][7]
- Further treatments, in 20 treatment increments, will be determined by that examination and in consultation with the referring physician.
- Rarely are 60 treatments exceeded. (Requires utilization review)
HBOT treatment protocol for cystitis or proctitis for open wounds in an irradiated field - 2.0-2.5 ATA oxygen for 90-120 minutes of oxygen breathing (Table 1 or 3)
- Daily basis for 20-40 treatments
- 20 treatments are usually prescribed prior to any surgical procedure. If the surgical procedure is complex, then we prefer 30 treatments prior to surgery.
- After the operative procedure, the patient should receive 10 additional treatments (for a total of 30 or 40 treatments)
- Extensions to treatment as described above.
- Transcutaneous oximetry (TCOM) may be used to determine tissue oxygenation after 20 treatments. This is an indirect measure of increased vascular density. Oximetry values alone are not sufficient to dictate further HBOT treatment needs.
- After 20 treatments, If measurable signs of healing are present and periwound TCOM values reach 40 mm Hg, HBOT may be paused and the wound can be followed for continued healing.
- If measurable signs of healing are not present after the initial 20 treatments re-evaluate looking for an incorrect diagnosis, persistent/recurrent tumor, persistent smoking, or other confounding problems.
- Wound evaluation and photography weekly and as needed
- Evaluation of tympanic membranes pre- and/or post- HBOT as needed
- Smoking cessation is highly encouraged.
|
|
Follow-Up
|
|
|
Treatment Threshold
|
20 – 40 treatments; 60 treatments in rare cases. (Utilization review should be requested after 60 treatments.) |
|
Coding
|
Refer to the ICD-10 Guideline for the appropriate ICD-10 Code
|
|
Comments
|
- If diabetes is present, blood glucose should be checked within an hour prior to treatment and immediately post-HBOT by unit personnel.
- If petroleum based dressings and ointments are a necessary part of the surgical dressing, ensure that they are not exposed and are completely covered with a moistened 100% cotton airtight dressing.
|
Primary Sources: Whelan and Kindwall [8], Huang [1][9], National Baromedical Services [10]

Fig.1. Soft tissue radionecrosis. 55 year old woman status post radical debulking surgery due to malignant nerve sheath tumor on left anterior thigh, 6600 cGy of external beam radiation, with non-healing wound 8 months after debulking. By Worth E.R, M.D

Fig.2. Soft tissue radionecrosis. Patient underwent HBOT for 2 months (30 sessions). By Worth E.R, M.D

Fig. 3. Soft tissue radionecrosis. After initial 30 sessions of HBOT, patient underwent surgical wound coverage with vertical rectus flap, then 10 additional HBOT sessions. By Worth E.R, M.D
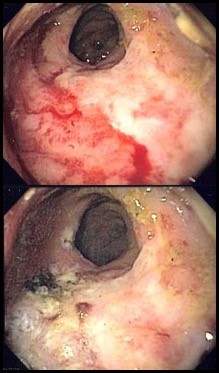 Fig. 4. Radiation proctitis. Top: pre-HBOT, with friable mucosa visible on the lower left. Bottom: post-HBOT (40 sessions), friable mucosa is absent. By Worth E.R, M.D
Fig. 4. Radiation proctitis. Top: pre-HBOT, with friable mucosa visible on the lower left. Bottom: post-HBOT (40 sessions), friable mucosa is absent. By Worth E.R, M.D
DOCUMENTATION
Radiation doses in excess of 40 Gray (4,000 cGy) are more commonly associated with compromised/delayed healing and persistent soft tissue/ integumentary breakdown within the previously irradiated field. These wounds often fail conservative wound management and/or surgical management. The role of hyperbaric oxygen is one of overcoming a hypovascular - hypocellular - hypoxic tissue bed and the late-radiation effects. Acute inflammatory responses to ongoing or recently completed radiation therapy need to be differentiated. The HBOT mechanism of action in soft tissue radiation Necrosis (STRN) is by stimulating angiogenesis, thereby overcoming the radiation-induced obliterative endarteritis. Below we explain in detail what needs to be documented and provide sample statements that can be adapted to suit your needs. See also:
History and Physical
- An initial assessment including a history and physical that clearly substantiates the condition for which HBOT is recommended.
- Prior medical, surgical and/or hyperbaric treatments.
- Past medical records must support a history of radiation therapy at the site identified by anatomical location.
Physical Exam
- Non-responding wound/ulcer within the previously irradiated field. We encourage you to be descriptive (e.g., "The non-healing breast wound is within the radiation tattoo marks on the lateral chest wall, and is located where the radiation oncologist noted peak radiation boost fields.")
- Often, the patients will have a 'radiation tattoo' mark near the wound/ulcer. Photograph the wound/ulcer and make reference to the demarcation by way of the tattoo.
- Use of HBOT often occurs in these cases by way of preparation for definitive coverage, whether flap or graft.
- There may be cases where a flap has been attempted and failed due to the hypoxic nature of tissue in the irradiated field. Describe the surgical procedure and denote a timeline of flap/graft failure after that surgery.
Impression
- Code First: Group 1 - Late Effects Radiation See ICD-10 Coding for STRN
- Group 2 - Anatomical Specific Radiation Codes See ICD-10 Coding for STRN
Plan
"For preventing wound healing complications in heavily irradiated tissue areas, we treat patients with 20 hyperbaric oxygen treatments at 2.0 or 2.4 ATA, breathing oxygen for 90 to 120 minutes. The patient then undergoes surgical repair followed by 10 or more treatments postoperatively, until the wound shows signs of continued healing. Should the patient already have a wound, 30 treatments are prescribed prior to any surgical procedure. We then treat 10 or more times postoperatively. For radiation cystitis/proctitis, we treat 30 times then have the referring physician examine the area under direct visualization. Further treatments, in 10 treatment increments, will be determined by that examination."
Additional comments to conclude the consultation may include:
“This patient has chronic radiation tissue injury consistent with delayed effects of ionizing radiation. This condition will be treated with hyperbaric oxygen therapy in conjunction with appropriate surgical repair or intervention.”
Risk and Benefit of Hyperbaric Oxygen Treatment
Indication for Hyperbaric Oxygen (HBO) Therapy
"Delayed effects of radiation are a complication of modern radiotherapy that can be well treated with hyperbaric oxygen therapy. Some examples of delayed radiation effects include soft tissue radionecrosis, osteoradionecrosis, radiation cystitis, radiation proctitis, and laryngeal chondroradionecrosis. The basic pathophysiology of delayed radiation tissue damage is endarteritis with resultant tissue hypoxia and secondary fibrosis.
Delayed radiation complications are often manifest as non-healing wounds located in previous irradiated areas and are precipitated by an additional insult such as surgery or trauma within the field of radiation. Hyperbaric oxygen has been shown to induce neovascularization and increase cellularity in irradiated and other hypoxic tissues. The success with randomized controlled studies in patients with mandibular osteoradionecrosis has led to successful use of hyperbaric oxygen in other body areas affected by radiation. Dental extractions or other surgical procedures are fraught with high complication rates when performed in heavily irradiated tissues without the benefit of preoperative hyperbaric oxygen therapy."
Sample Order
Documentation by Certified Hyperbaric Nurse and Certified Hyperbaric Technician
The certified hyperbaric technician (CHT) and certified hyperbaric nurse (CHRN) should maintain an accurate record of the care and related support services delivered during each patient’s course of hyperbaric oxygen therapy. The patient's chart is a legal document and as such, must reflect in meaningful terms the patient's condition, progress, and care rendered. The provider and nurse's notes must be concise, accurate, and support medical necessity for the treatment ordered. The notes must reflect responsibility for the care rendered. For details, see topic "Documentation: Hyperbaric Treatment Notes by the CHRN and CHT"
Daily treatment should include, but is not limited to the following:
- Physician Order - confirm daily HBO treatment order.
- Patient Assessment (by the CHRN or CHT)
- Pre-treatment Safety Check (by the CHRN or CHT)
- Documentation of the Treatment Log (by the CHRN or CHT)
- Physician Supervision (by the CHRN or CHT)
- Care Provided (by the CHRN or CHT)
- Plan of Care (by the CHRN or CHT, based on physician orders)
CLINICAL EVIDENCE AND RECOMMENDATIONS
-
1A
For patients with refractory radiation proctitis with a history of radiation treatment terminating at least 6 months prior to onset of signs and symptoms, we recommend HBOT as an adjunctive therapy to improve healing responses (as demonstrated by SOMA-LENT scores) (Grade 1A)
-
1B
For patients who need reconstructive soft tissue surgery or flaps into a previously irradiated area in the head or neck, we recommend HBOT therapy to prevent postoperative wound dehiscence (Grade 1B) - 1CFor patients with hemorrhagic radiation cystitis with a history of radiation treatment terminating at least 6 months prior to onset of signs and symptoms, we recommend HBOT as an adjunctive therapy to resolve bleeding (Grade 1C).[11]
-
2C
For patients with hemorrhagic radiation cystitis with a history of radiation treatment terminating at least 6 months prior to onset of signs and symptoms, we suggest HBOT as an adjunctive therapy to resolve bleeding (Grade 2C)
-
2C
For patients with radiation-induced lesions of the larynx with a history of radiation treatment terminating at least 6 months prior to onset of signs and symptoms, we suggest HBOT as an adjunctive therapy to promote healing of the radio-induced lesions (Grade 2C).
-
-
Rationale: The impact of HBOT in terms of its beneficial effects is likely to involve all three of these mechanisms in irradiated tissues: HBOT stimulates angiogenesis and secondarily improves tissue oxygenation; reduces fibrosis; and mobilizes and induces an increase of stem cells within irradiated tissues.[1][9] For people with soft tissue radiation necrosis affecting tissues of the head, neck, bladder and rectum, HBOT may be associated with improved outcomes.[9] Quality of evidence varies according to the type of irradiated soft tissue being treated. Of note, high-certainty evidence derived from a well-designed randomized clinical trial supports the use of HBOT to treat radiation proctitis [12]; and moderate-certainty evidence supports the use of HBOT pre- and postoperatively to prevent wound dehiscence following head and neck soft tissue reconstruction in previously irradiated areas.[13] Evidence supporting use of HBOT to treat hemorrhagic cystitis and radiation-induced lesions of the larynx is of low-certainty, mainly supported by observational studies.[9]
- Utilization of resources: for patients with radiation cystitis, adjunctive HBOT has been found to be a cost-effective intervention. A retrospective study analyzing Medicare claims of patients with radiation cystitis treated with adjunctive HBOT showed a 36% reduction in urinary bleeding, a 78% reduced frequency of blood transfusion for hematuria, a 31% reduction in endoscopic procedures, and fewer hospitalizations when study patients were compared to control. When at least 40 treatments were provided, cost savings per patient increased to $11,548 for the HBOT study group compared to the control group, representing a 37% reduction in Medicare spending for the HBOT-treated group.[11]
- Despite potential benefits, a frequent concern is the fear that HBOT will somehow accelerate malignant growth or cause a dormant malignancy to be reactivated. However, an overwhelming majority of both clinical reports, animal studies, and plated cell cultures showed no enhancement of cancer growth.[1] The patient should be informed of the possible risks and complications of hyperbaric oxygen therapy. The standard risks and benefits for HBOT have been discussed and listed here.
- Medicare coverage: Medicare covers preoperative and postoperative use of HBOT as an adjunctive therapy for existing soft tissue radionecrosis. Prerequisite for treatment includes history of radiation treatment to the region of the documented injury, terminating at least 6 months prior to onset of signs or symptoms or planned surgical intervention at the site.[1] See section on 'Coverage and Reimbursement' below.
OPERATIONAL CONSIDERATIONS
Providing HBOT in a safe manner is the primary objective with each and every treatment. The clinical team (physician, CHT, CHRN, etc) providing HBOT goes to great lengths to ensure patient safety with every treatment. A summary of operational considerations pertaining to adjunct HBOT for soft tissue radiation necrosis is provided below:
Chamber Inspections
- Routine chamber inspections should be conducted to confirm chamber maintenance procedures and the safe operation of all equipment utilized during HBOT.
- To ensure the safety of the environment in the hyperbaric medicine facility, chamber inspections are to be performed routinely (i.e. daily, monthly, semi-annually, as needed). Processes and systems that meet standards set forth by The Joint Commission (TJC) and the Undersea and Hyperbaric Medical Society (UHMS) should be utilized, and elements that have been developed within the field (in some cases through “near misses”) may be incorporated. These processes and systems can be implemented through customized patient-centered checklists. Checklists have a wide range of applications, with the potential to improve patient education, pre-procedure planning, discharge instructions, care coordination, chronic care management, and plans for staying well.
- For resources on chamber inspections, see topic "HBO Safety Inspections".
Ground testing
- NFPA 99 requires that all hyperbaric chambers are grounded and patients inside chambers filled with 100% oxygen are likewise grounded. Wrist continuity tests prior to each treatment and daily chamber checks including chamber stud to wall measurements and patient ground jack to chamber stud measurements ensure ongoing continuity.
Prohibited Item(s), Assessment and Authorization
- Wound dressings, devices, and other objects that go in the hyperbaric chamber with the patient may raise important safety concerns, including the production of heat, production of static electricity, production of flammable vapor, ignition temperature, and total fuel load. It is critical that clinicians understand which dressings, devices, and objects are prohibited, restricted or allowed inside a hyperbaric chamber during HBOT for soft tissue radiation necrosis.
- Frequently, questions arise in regard to which items are prohibited, restricted or allowed inside a hyperbaric chamber during HBOT. The NFPA 99 2018 edition, chapter 14 "Hyperbaric Facilities", provides the process for effectively managing patient care product(s) during HBOT. The NFPA 99 2018 edition - 14.3.1.6.4.4 states “Physician and Safety Director approval to use prohibited items shall be stated in writing for all prohibited materials employed”. [14]
- Each hyperbaric facility should maintain an internal list of items that are approved for use, should be used with caution and should not be used in the chamber. An authorization form is required for items that should be used with caution. To facilitate assessment, clinicians might opt to utilize the Go-No-Go Risk Assessment Tool. The tool is an interactive process that enables hyperbaric technicians, Safety and Medical Directors to document the product information necessary to complete the risk assessment process. Upon completion of the process, the user will have the ability to print or email the document. In addition, clinicians can review lists of items that are approved for use, should be used with caution and should not be used in the chamber. See " Go-No-Go Lists / Prohibited Items" and "Go-No-Go: Frequently Asked Questions".
Ancillary Equipment
- All equipment utilized by the hyperbaric medicine facility is maintained through a program of regular preventative maintenance. The manufacturer maintains the hyperbaric chambers during the regularly scheduled service contract. Ancillary equipment (e.g. cardiac monitor leads, TCOM sensors) should be serviced by the Hospital's Biomedical Department and maintained in accordance with the recommendations of the manufacturer. See topics "Ear Exam - Barotrauma" and "Ancillary Equipment".
Air Breaks
- During HBOT for soft tissue radiation necrosis, it is necessary to provide an alternative air breathing source. This may also be necessary to reduce the risk of central nervous system oxygen toxicity. The air breathing system consists of an independent high-pressure air source, capable of providing flow that is sufficient to meet the patient's inspiratory demand. Air breathing systems may be provided by institutional gas outlet (wall outlet) or via portable "H" cylinders utilizing a diameter index safety system (DISS) regulator. Delivery of the air break to the patient may be provided by disposable non-rebreather mask, demand valve and resuscitation mask or trach collar. For purposes of infection control, masks should be single patient use and cleaned or replaced (per patient) as needed.
- While the use of air breaks to decrease the incidence of CNS oxygen toxicity has not been directly demonstrated, there is a large amount of published data on the cause of oxygen toxicity related directly to a combination of the level of FiO2, and time. As such, these air breaks limit the interval time exposure and are expected to decrease the risk of oxygen toxicity. [15]
Infection Control - Cleaning/ Disinfection of the Hyperbaric Chamber
- The cleaning and disinfection of acrylic monoplace chambers is done with caution because many commercial biohazard-cleaning agents contain alcohol. While alcohol is adequate to kill many pathogens, it is destructive to acrylic and can produce flammable fumes and vapors creating a fire hazard in the chamber and the immediate area. Therefore, only manufacturer-approved cleaning products are used for disinfection of the hyperbaric chamber and accompanying equipment. Particular cleaning and disinfecting tasks are divided among staff from environmental services, equipment or biomedical device services, respiratory services, nursing, and other departments of the health care team.
- Adverse outcomes related the risk of infection stands at the forefront of concern for patients with soft tissue radiation necrosis. Particular attention should be given to cleaning and disinfection of the hyperbaric chamber acrylic, stretcher and associated equipment, including observing the specific kill times of the solution used prior to the delivery HBOT. See topic: "Cleaning and Disinfection of Hyperbaric Oxygen Monoplace Chamber"
Barotrauma
- Assessment of the patient and their past medical history is necessary to identify and minimize the risk of barotraumas. If the patient has history of sinus, tooth, and ear problems, compress slowly and observe patient for signs of pain.
- Middle-ear barotrauma: The most common type of barotrauma experienced by patients receiving HBOT is middle-ear barotrauma (MEB). Normally, the middle ear is a closed, vascular lined space and therefore subject to pressure change. The normal means by which the middle ear remains at an equal pressure with the surrounding tissue is through the opening of the Eustachian tube. During descent, the increasing pressure of the surrounding water leads to “middle-ear squeeze.” If a patient is suffering from Eustachian tube dysfunction, he or she likely will be unable to equalize and will subsequently develop middle-ear barotrauma. [8]
- Pneumothorax: A complete and accurate pulmonary assessment is essential to avoid or prevent gas expansion problems. Assessing the patient with a significant pulmonary history is a key starting point. Identify any history of asthma, chronic obstructive pulmonary dysfunction (COPD), fibrosis, spontaneous pneumothorax, or chest trauma.
- The absolute contraindication for HBOT is the unvented pneumothorax.
- Signs and symptoms of pneumothorax include: Sudden shortness of breath, Sudden stabbing chest pain, Tracheal shift to affected side in cases of tension, Asymmetrical chest movement (lack or reduced chest excursion on affected side), Increase in respiratory distress with decompression, with relief on recompression. [8]
Blood Glucose Level and HBOT
- It is necessary to ensure that all patients who are currently being treated for irregular blood glucose levels do not experience a hypoglycemic event as a result of ongoing HBOT. Most studies suggest that blood glucose decreases in patients with diabetes who undergo HBOT. This decrease in blood glucose is estimated at 50 mg/dl. HBOT might not be as effective in patients with non-insulin dependent diabetes mellitus patients, compared to patients without diabetes. [8]
- If diabetes mellitus is present, blood glucose should be checked within 1 hour prior to treatment and immediately post-HBOT. The goal is to ensure that all patients who are currently being treated, do not experience a hypoglycemic event as a result of ongoing HBOT. Hypoglycemia in the hyperbaric environment may present similar symptoms as oxygen toxicity, including but not limited to sweating, pale skin, shakiness, anxiety, tingling or numbness of the tongue or cheek. See section 'Blood Glucose Level and HBOT' in topic "Patient Care".
Medications in the hyperbaric environment
- The hyperbaric environment creates numerous considerations for the use of drug therapies within it. Physiologic changes to the body due to HBOT may lead to pharmacokinetic changes in drug disposition. In addition, HBO acting as a drug can interact and enhance or lessen the physiologic effect of the drug. Most drugs will not interact unfavorably with oxygen. Unless specific contraindications or precautions have been addressed, it is generally safe to assume a medication can be used. [8] Pharmacodynamic interactions result in modification of the pharmacologic effect of the drug after administration. These interactions will increase or decrease the effects of oxygen or the drug. [8]
- Patients receiving antibiotics with elastomeric infusion pumps (also known as "space balls") may continue to receive antibiotics in the chamber, however infusion amounts during changes of atmospheric pressure should still be monitored. If the pump is full of air, then it may not provide standardized infusion rate. A study shows that the antibiotic flow rate for ceftazidime 6 g is not significantly affected by increases in ambient pressure across the pressure range of 101.3 kPa to 284 kPa. However, there was evidence that the specific antibiotic solution might affect flow rates and this requires further study.
- For potential interactions of drugs administered to patients with soft tissue radiation necrosis, see topic "Medications In The Hyperbaric Environment".
Oxygen Toxicity
- The hyperbaric staff should be skilled in reducing the potential for and management of oxygen toxicity for the patient receiving HBOT.
- Central Nervous System (CNS) oxygen toxicity can occur in patients breathing oxygen at pressures of 2.0 ATA (atmosphere absolute) or greater. Convulsions may occur abruptly or may be preceded by other signs of central nervous system irritability.[8] Early estimates of the seizure rate during therapeutic oxygen exposures at 2-3 ATA reported a convulsion incidence of about one per 10,000 therapies or 0.01%. [8]
- The hyperbaric physician will be notified immediately if a patient experiences signs or symptoms of oxygen toxicity during HBOT.
CNS toxicity
- Observe patient closely for premonitory signs and symptoms of CNS Oxygen Toxicity such as:
- V : vision-visual changes, blurred vision, visual hallucinations
- E : Ears- Auditory hallucinations, ringing in the ears
- N : Nausea- May include emesis
- T : Twitching- Restlessness, numbness, focal twitching (note time, duration and site)
- I : irritability- Change in personality
- D : Dizziness- Vertigo
- C : Convulsions- Seizure activity
- C : Change in mentation - Change in affect or of a non-descriptive complaint like, “I just don’t feel right” [16]
Pulmonary Oxygen Toxicity
- Most current applications of HBOT do not cause pulmonary symptoms or clinically significant pulmonary functional deficits. [17] Prolonged exposure to oxygen pressures greater than 0.5 ATA is associated with the development of intratracheal and bronchial irritation. Pulmonary oxygen toxicity is not expected from routine daily HBOT. The possibility of development does exist with prolonged exposure most typically related to long treatment tables such as US Navy Treatment Table 6 used for decompression illness, but even these cases would be mild and self-limiting.[18]
- Continued oxygen exposure may lead to impaired pulmonary function and eventually acute respiratory distress syndrome (ARDS). Symptoms include:
- Substernal burning,
- Chest tightness
- Cough
- Dyspnea
- These changes are seen over the course of days to weeks at lower oxygen pressures and occur more rapidly as the oxygen pressure is increased.[8]
Ocular Oxygen Toxicity
- Vision changes as a side effect of HBOT have been observed in patients undergoing prolonged periods of daily HBOT. The rate of these changes has been reported in the literature to be ∼0.25 diopter per week and progressive throughout the course of ongoing treatment. Myopia has been reported in 25–100% of patients undergoing HBOT after several weeks at pressures of 2.0 ATA and greater.[18] When providing HBO for the patient being treated for soft tissue radiation necrosis it is important to discuss the risks, hazards and potential side effects with the patient and family. Documentation of this discussion and patient/ family's understanding should be clearly stated in the patient record. For further information See topic:"Hyperbaric Oxygen Therapy and Visual Acuity"
NURSING INTERVENTIONS
Nursing interventions that are relevant for adjunct HBOT of soft tissue radiation necrosis are presented below. [19] For further information see topic "Nursing Interventions".
Knowledge deficit related to hyperbaric oxygen therapy and treatment procedures
- Assess and document the patient and/or family's understanding of purpose and goals of hyperbaric oxygen therapy (HBO), procedures involved, and potential hazards of HBO.
- Utilize the teach-back method to confirm patient understanding and identify and address barriers to learning. Involve an interpreter if indicated, apply age-specific teaching, consider cultural/religious factors, assess readiness to learn, and identify patient's expectations of treatment.
- See section 'Knowledge deficit related to hyperbaric oxygen therapy and treatment procedures' in topic "Nursing Intervention"
Anxiety related to hyperbaric oxygen treatments or other medical problems
- Assess the patient for a history of confinement anxiety and implement preventative measures as appropriate. It is important to reinforce to patient that someone will always be with them, and the staff are well trained for emergency procedures. Identify signs of symptoms of anxiety before and during HBO treatment such as:
- Patient states anxiety
- Tense-appearing facial/body posturing
- Complaint of nausea or diarrhea
- Feelings of being confined or smothered
- Defensive or argumentative attitude
- Hyperventilation
- Diaphoresis and hyperventilation
- Tachycardia
- Restlessness
- Sudden feeling of being hot
- See section 'Anxiety related to hyperbaric oxygen treatments or other medical problems' in topic "Nursing Intervention"
Potential for injury within the hyperbaric facility related to transferring the patient in and out of the chamber
- When transferring a patient that is being treated for soft tissue radiation necrosis, comply with the facility's fall risk prevention policy. Prior to transfer of the patient assess fall risk and safety precautions. Communicate and involve patient with the plan of action and provide patient education regarding safety precautions. Provide assistance with transfers as patient needs apply to ensure compliance with institutional/facility policy.
Potential for injury related to fire within the hyperbaric chamber
- Fuel sources in an oxygen-enriched environment are an unavoidable circumstance of HBOT and include linens, equipment, dressings, and the patient. The fire triangle consists of oxygen, fuel, and an ignition source (heat). In HBOT an ignition source is needed to complete the fire triangle. This may occur due to a spark in the chamber. Follow facility fire prevention steps and NFPA chapter 14 probes for Class A and Class B hyperbaric chambers. HBOT teaching and consent should include the risks of fire in the chamber. Provide the patient and family with written instructions regarding the risk of prohibited materials during HBOT. Prior to each hyperbaric treatment, staff should perform and document the pre-treatment safety checklist. Ensure this has been performed and time-stamped prior to descent. Patients receiving treatment for soft tissue radiation necrosis may have surgical dressings that are ordered to remain intact. A risk assessment per the Safety Director in collaboration with the Medical Director to determine if they may enter the chamber on a case by case basis. Safety measures should be initiated if the risk assessment allows for item to enter the chamber as well as completion of a prohibited item's authorization form signed by the Safety and Medical Directors.
Potential for injury related to changes in atmospheric pressure within the hyperbaric chamber
- Assess patient's and inside attendant's knowledge of ear clearing techniques and ability to equalize pressure. Collaborate with provider to assess tympanic membrane (TM) for suspected barotrauma prior to and after the first HBO treatment and per patient complaint. Collaborate with the provider to describe and document observations including color and visibility of TM, presence of wax, blood/fluid/air and any hearing deficits or changes. Methods to equalize pressure in the middle ear during HBO treatment include: yawning, swallowing, jaw thrust, head tilt, Valsalva, Toynbee, Roydhouse, Frenzel, etc. Reinforce the importance of notifying the chamber operator immediately when pressure or fullness is felt in the middle ear.
Potential for unstable blood glucose level related to hyperbaric oxygen therapy and disease pathology
- Literature notes hyperbaric oxygen therapy carries its own mechanism for increased glucose usage through oxygen-mediated transport of glucose into muscle cells and may also increase insulin sensitivity. Prevention of acute hypoglycemia in the hyperbaric chamber is vital for patient safety. Follow facility policy and procedure guidelines for pre and post-treatment glucose control. Prior to treatment assess the patient's knowledge level, recent hypoglycemic events, and patient-specific symptoms of hypoglycemia. Proper glucose control < 200mg/dL is vital for wound healing. Consider timing of short and long-acting glycemic control medications when scheduling HBO to avoid peak action time while at depth in the chamber.
CODING
COVERAGE AND REIMBURSEMENT
- Medicare covers preoperative and postoperative use of HBOT as an adjunctive therapy for existing soft tissue radionecrosis. Prerequisite for treatment includes history of radiation treatment to the region of the documented injury, terminating at least 6 months prior to onset of signs or symptoms or planned surgical intervention at the site.[1]
- Numerous forms of soft tissue radiation necrosis and treatment with HBOT have been documented with beneficial effects. Tissues previously irradiated with subsequent planned surgery appear to benefit from HBOT surrounding the surgery with decreased morbidity from large vessel necrosis. For this reason patients manifesting signs and symptoms of radiation injury will be approved for coincidental HBOT, without the histologic diagnosis of ongoing osteoradionecrosis or soft tissue radionecrosis.[20]
- Regarding Radiation Proctitis, a recent article on the UHMS website entitled UHMS Member Alerts the Society on Problems with CMS Coverage of Radiation Proctitis: "The Case of the Disappearing Indication" written by Tom Bozzuto, DO, FACEP, FFACHM, UHM addresses an Ask the Contractor Teleconference (ACT) with Palmetto GBA. Dr. Leland Garrett, Medical Director of Palmetto GBA, Columbia South Carolina stated that radiation proctitis is not a covered indication under Soft tissue radiation injury as the bowel is not considered soft tissue. The only provider option available to have these claims reconsidered for payment would be the Medicare appeal process. It is imperative that providers are knowledgeable of their Local Coverage Determinations for hyperbaric oxygen therapy before proceeding with treatment.[21]
- Utilization Review should be accomplished after 60 treatments when HBOT is applied to the treatment of radiation injury. Characteristically, most treatment courses for radiation injury will be in the range of 30-60 treatments when the course of treatment is carried out with daily treatments at 2.0-2.5 ATA of 100% oxygen for 90-120 minutes. [9]
- One caveat exists regarding the type of radiation used to treat certain cancers. We are aware of several institutions using neutron beams rather than the more common electron beam radiotherapy. Neutrons are heavy particles in comparison and have a surprisingly larger soft tissue radiation injury. Because of the particle size and collateral damage, these patients may require more than 60 treatments before wounds heal. We have seen this in several cases of head/neck and prostate radiation.
APPENDIX
Summary of Evidence
We reviewed the guidelines and studies published since guidelines were last updated. Applying the GRADE framework to the combined body of evidence, we found that the use of HBOT to:
- Treat patients with hemorrhagic radiation cystitis is supported by low-certainty evidence (evidence level C) derived from observational studies and case series [9]
- Prevent postoperative wound dehiscence in patients who undergo soft tissue reconstruction in the head and neck area after radiation, is supported by moderate-certainty evidence derived from a 2016 Cochrane meta-analysis [13]
- Treat patients with refractory radiation proctitis (as demonstrated by improvement in SOMA-LENT scores) is supported by high-certainty evidence derived from a large RCT at low risk of bias conducted by Clarke et al. [12]
- Treat patients with radiation-induced lesions of the larynx is supported by low-certainty evidence derived from observational studies and case series [9]
- A large, retrospective review in Australia showed response for STRN and HBOT of 95% (proctitis), 85% (cystitis), and 84% (other body soft tissues). The HBOT complication rate was 10.6% (ear barotrauma), 4.2% (reversible myopia), 0.5% (dental barotrauma), and 0.5% (myocardial infarction) from 276 consecutive patients. [22]
Systematic reviews:
- A 2023 systematic review by Cochrane aimed to evaluate the benefits and harms of hyperbaric oxygen therapy (HBOT) for treating or preventing late radiation tissue injury (LRTI) compared to regimens that excluded HBOT. The study included 18 studies (n=1071 participants). HBOT may not prevent death at one year (risk ratio (RR) 0.93, 95% confidence interval (CI) 0.47 to 1.83; I2 = 0%; 3 RCTs, 166 participants; low-certainty evidence). There is some evidence that HBOT may result in complete resolution or provide significant improvement of LRTI (RR 1.39, 95% CI 1.02 to 1.89; I2 = 64%; 5 RCTs, 468 participants; low-certainty evidence) and HBOT may result in a large reduction in wound dehiscence following head and neck soft tissue surgery (RR 0.24, 95% CI 0.06 to 0.94; I2 = 70%; 2 RCTs, 264 participants; low-certainty evidence). In addition, pain scores in ORN improve slightly after HBOT at 12 months (mean difference (MD) -10.72, 95% CI -18.97 to -2.47; I2 = 40%; 2 RCTs, 157 participants; moderate-certainty evidence). Regarding adverse events, HBOT results in a higher risk of a reduction in visual acuity (RR 4.03, 95% CI 1.65 to 9.84; 5 RCTs, 438 participants; high-certainty evidence). There was a risk of ear barotrauma in people receiving HBOT when no sham pressurization was used for the control group (RR 9.08, 95% CI 2.21 to 37.26; I2 = 0%; 4 RCTs, 357 participants; high-certainty evidence), but no such increase when a sham pressurization was employed (RR 1.07, 95% CI 0.52 to 2.21; I2 = 74%; 2 RCTs, 158 participants; high-certainty evidence). Authors concluded that studies suggest that for people with LRTI affecting tissues of the head, neck, bladder and rectum, HBOT may be associated with improved outcomes (low- to moderate-certainty evidence). HBOT may also result in a reduced risk of wound dehiscence and a modest reduction in pain following head and neck irradiation. However, HBOT is unlikely to influence the risk of death in the short term. HBOT also carries a risk of adverse events, including an increased risk of a reduction in visual acuity (usually temporary) and of ear barotrauma on compression.[23]
- A 2016 systematic review [24] included 8 studies (1 uncontrolled observational cohort, 5 case series, and 2 case reports) including 720 participants who received HBOT for radiation induced skin necrosis.[25][26][27][28][29][30][31][32] Sites of skin necrosis included lower extremity, buttocks , scrotum, abdomen, chest wall, upper extremity, and head and neck. Majority of studies were at high risk of bias. Six studies provided the primary outcome measure of interest: complete wound healing after HBOT (98 patients). Pooled together the rate of complete wound healing was 79.6% (78/98). Two studies provided the secondary outcome measures of interest, symptomatic improvement of skin necrosis after HBOT (622 patients). Pooled together the rate of symptomatic improvement was 86% (535/622). Further analysis revealed the rate of complete resolution of pain symptoms was 30% (187/6 22), wound healing symptoms 30% (187/622), and wound drainage symptoms 39%(243/ 622). Evidence level is considered as low certainty (evidence level C) as currently no randomized control trial has tested the efficacy of HBOT in the treatment of skin necrosis due to late radiation tissue injury. Authors concluded that HBO is a safe intervention with promising outcomes, however additional evidence is needed to endorse its application as a relevant therapy in the treatment of radiation induced skin necrosis.
- A 2016 Cochrane systematic review [13] included 14 trials (753 participants) that assessed the effect of HBOT on complete mucosal cover in people with osteoradionecrosis and on wound healing of dehiscence following complex head and neck surgery and irradiation. 2 RCTs (264 participants) assessed soft tissue radiation injuries and showed that HBOT is effective in promoting healing of dehiscence following complex head and neck surgery and irradiation (moderate quality evidence, RR 4.23 95% CI, (1.06 to 16.83) of from single studies there was a significantly increased chance of improvement or cure following HBOT for radiation proctitis (RR 1.72; 95% CI 1.0 to 2.9, P value = 0.04, NNTB 5). Authors concluded that these small trials suggest that for people with LRTI affecting tissues of the head, neck, anus and rectum, HBOT is associated with improved outcome.
Guidelines:
- The UHMS Hyperbaric Oxygen Therapy Indications 15th edition[1] and the 2017 European Committee for Hyperbaric Medicine Guidelines support the use of HBOT as therapy to treat Soft Tissue Radiation Necrosis, and although the guidelines use different evidence grading methodologies, they are in agreement regarding strength of recommendation.[9][33] See table below:
|
HBO therapy for Soft Tissue Injury
|
UHMS, 2023
|
ECHMG, 2017
|
|
Treatment of soft tissue injury
|
AHA Level Ib
|
n/a
|
|
Treatment of hemorrhagic radiation cystitis
|
n/a
|
Grade 1B
|
|
Treatment of radiation proctitis
|
n/a
|
Grade 1A
|
|
The treatment of soft-tissue radionecrosis (other than cystitis and proctitis), in particular in the head and neck area
|
n/a
|
Grade 2C
|
|
Treating or preventing radio-induced lesions of the larynx
|
n/a
|
Grade 3C
|
Randomized Clinical Trials
- In 2024, Dieuwke et al, conducted an RCT in the Netherlands (n= 189 patients) to assess effectiveness of HBOT for late local toxic effects in women who received adjuvant radiotherapy for breast cancer. Among patients who completed HBOT, a significant reduction in pain and fibrosis was observed. A smaller than anticipated proportion of women with late local toxic effects was prepared to undergo HBOT.[34]
- In 2008, Clarke et al conducted an RCT with 120 evaluated participants that compared the effects of HBOT on the late effects normal tissue-subjective, objective, management, analytic (SOMA-LENT) score and standardized clinical assessment in patients with chronic refractory radiation proctitis [12]. In the experimental group, the mean was lower (p = 0.0150) and the amount of improvement nearly twice as great (5.00 vs. 2.61, p = 0.0019). Similarly, Group 1 had a greater portion of responders per clinical assessment than did Group 2 (88.9% vs. 62.5%, respectively; p = 0.0009). Significance improved when the data were analyzed from an intention to treat perspective (p = 0.0006). Authors concluded that HBOT significantly improved the healing responses in patients with refractory radiation proctitis, generating an absolute risk reduction of 32% (number needed to treat 3) between the groups after the initial allocation. The study is considered by the 2016 Cochrane systematic review [13] as at low risk of bias (evidence level A).
Observational Studies
- Case series support use of HBO to resolve hemorrhagic radiation cystitis.[9] (level C)
- In 2024, Feldmeier et al. published a retrospective study analyzing Medicare claims of patients with radiation cystitis treated with adjunctive HBOT showed a 36% reduction in urinary bleeding, a 78% reduced frequency of blood transfusion for hematuria, a 31% reduction in endoscopic procedures, and fewer hospitalizations when study patients were compared to control. When at least 40 treatments were provided, cost savings per patient increased to $11,548 for the HBOT study group compared to the control group, representing a 37% reduction in Medicare spending for the HBOT-treated group. Authors concluded that HBOT is a cost-effective adjunctive treatment for patients with radiation cystitis. [11]
CATEGORY A CONTINUING EDUCATION CREDIT
This topic has been reviewed and approved by the National Board of Diving and Hyperbaric Medical Technology (NBDHMT) for one (1) Category A Credit. 'Meeting the Category A requirement related directly to any combination of hyperbaric operations, related technical aspects and chamber safety.'
To claim the credit:
- 1. Read the topic
- 2. Answer the examination and course critique questions.
- 3. Receive the certificate by e-mail. A passing score of 70% is required (please allow up to 8 business days for processing)
For more information on Category A continuing education credits see blog post " Hyperbaric Certification and Continuing Education for Technicians & Nurses".
REVISION UPDATES
| Date | Description |
| 6/4/24 | Updated section 'Clinical Evidence and Recommendations', updated references |
| 4/14/23 | Updated 'Hyperbaric criteria', updated references |
| 5/21/21 | Added sections 'Category A Continuing Education Credit' |
| 12/31/20 | Added sections ‘Documentation by Certified Hyperbaric Nurse and Certified Hyperbaric Technician’, ‘Operational Considerations’, ‘Nursing Interventions’, updated references |
5/21/19
| Added figures |
| 4/15/19 | Added section on Coverage and Reimbursement |
Official reprint from WoundReference® woundreference.com ©2025 Wound Reference, Inc. All Rights Reserved
NOTE: This is a controlled document. This document is not a substitute for proper training, experience, and exercising of professional judgment. While every effort has been made to ensure the accuracy of the contents, neither the authors nor the Wound Reference, Inc. give any guarantee as to the accuracy of the information contained in them nor accept any liability, with respect to loss, damage, injury or expense arising from any such errors or omissions in the contents of the work.