ABSTRACT
A wound is a break in the continuity of a bodily tissue, such as the skin or mucous membrane.[1] Wounds can be caused by events that are external to the organism - such as trauma, burns, or surgical incisions; and wounds can also be of endogenous origin - such as a distal ischemic event involving the toes due to embolism or arterial stenosis.
Wound attributes, such as its causative mechanism, size, depth and location are useful for characterizing its type.[2] When a wound is being assessed, it is also important to determine the stage of wound healing, extent of tissue repair, presence of any obvious elements preventing complete wound closure, and the patient's psychological status. Complete restoration of tissue integrity requires multidisciplinary care and patient adherence to the recommended treatment.[2]
The patient's baseline clinical condition greatly influences the wound healing process. Healthy individuals tend to recover quickly, with restoration of skin integrity and scars that have a better appearance as well as fewer complications. Patients with chronic diseases (e.g. diabetes mellitus and hypertension, malnutrition or obesity) tend to present delayed wound healing and have greater risk of complications such as infection, and functional and psychological sequelae.[3][4]
However, even in healthy patients, the normal response to tissue repair may not take place adequately. In such cases, wounds may undergo a hypoproliferative process, resulting in atrophic or wide scars. Wounds may also undergo a hyperproliferative process, with excessive formation and deposition of connective tissue resulting in hypertrophic scars and keloids.[5]
This topic reviews the different wound types (e.g. acute and chronic, partial and full-thickness, etc), wound healing phases, pathophysiology of chronic wounds, biofilm, and pathological scarring. For a review on function, structure, and cells of the skin see topic “The Skin”.
INTRODUCTION
Overview
This topic reviews principles of wound healing and provides updates on wounds from various perspectives - economic, physiological and pathological. To better understand the wound healing process though, it is important to first understand the characteristics of the skin as an organ. For a review on function, structure, and cells of the skin see topic “The Skin”.
Background
-
Definitions:
-
Wound: a wound is a disruption in the continuity of a tissue, such as the skin or mucous membrane. Wounds may be categorized as acute or chronic. From a medical coding perspective, the term “wound” refers to an acute wound (e.g. surgical wound, traumatic wound, etc).[6]
-
Ulcer: the term "ulcer" is often used interchangeably with “wounds”. From a medical coding perspective however, “ulcer” refers to a chronic wound (e.g., pressure ulcer/injury, venous leg ulcer, diabetic foot ulcer, etc).[6]
-
Relevance
- Wound management is a significant burden for healthcare services, since it consumes a great amount of financial and human resources.[7][8] Wounds have a considerable impact - frequently not recognized - on patients, caregivers and the health system itself, which explains why chronic wounds are also known as a “silent epidemic”.[9]
- Estimated treatment costs vary and depend on various factors related to the wound, complications and facility at which the patient is receiving care .[9]
- In the U.S., it is estimated that about US$ 32 billion are spent on chronic wounds per year.[10]
- In the United Kingdom, the financial burden of treating chronic and acute wounds of more than 650,000 patients by the National Health Service (NHS) was declared to be approximately £ 5 billion in 2015.[11]
- It is important to emphasize that all these epidemiological data and values are subject to various variations and subjectivities, and do not portray the full and complete picture of a patient with a wound, particularly if it is a chronic wound.[12] For a more representative analysis of the costs of treating wounds, it would be necessary to consider other issues - such as the frequency with which dressings are applied, what type of dressings are applied, who applies the dressing, the care setting where the dressing is applied, etc. [12] Studies have shown that the most expensive component of care - which is nevertheless of vital importance - is the care provided by medical personnel. [13]
-
Prevalence
- The prevalence of chronic wounds is estimated to be about 1.5 to 2 million people in Europe. In the U.S., chronic wounds affect about 6.5 million people.[9] Individuals aged 65 years or more account for at least 85% of cases.[9]
TYPES OF WOUNDS
Acute and chronic wounds
- From a clinical standpoint, wounds may be classified according to the time interval over which they remain open, that is, by the time interval that has gone by without complete reepithelialization:
-
- Acute wounds (Figure 1): acute wounds are those that heal through in a timely fashion, and undergo the wound healing phases of inflammation, cell proliferation and tissue remodeling.
-
Chronic wounds (Figure 2): on the other hand, chronic wounds fail to proceed through the normal phases of wound healing in an orderly or timely manner, often remaining in a stage of chronic inflammation.[14] Literature varies, but in general, chronic wounds are defined by wounds that fail to heal within 4 weeks to 3 months.[15] In chronic wounds, the wound healing process is protracted, incomplete and disorganized, resulting in anatomical and functional alterations. In spite of a variety of therapeutic strategies that have been suggested to optimize wound healing over recent decades, the effective treatment of chronic wounds remains a challenge. Acute wounds may become chronic in patients with co-morbidities and risk factors which impair wound healing, such as mobility impairment, chronic venous hypertension, uncontrolled diabetes and malignant neoplasms.
- For other differences between acute and chronic wounds, see Table 1 below.
- From a medical coding standpoint, wounds are classified as acute or chronic according to their etiology; there is no timeline during which an acute wound turns into a chronic ulcer.[6] For instance, traumatic wounds, surgical wounds are considered acute wounds, and pressure ulcers and non-pressure ulcers, varicose veins with ulcers, etc, are considered chronic wounds or ulcers.
Table 1. Comparison of acute and chronic wounds [16]
| Acute wound |
Chronic wound |
|

Fig. 1. Traumatic wound (example of acute wound)
|

Fig. 2. Sacral pressure ulcer/injury (example of chronic wound)
|
- Healing occurs in a timely fashion. The wound undergoes the wound healing phases of inflammation, cell proliferation and tissue remodeling.
- Exudate is rich in endogenous proteases, which contribute to the proliferation and growth of new cells, facilitating wound closure. Matrix metalloproteinase (MMP) activities are inhibited by the presence of MMP inhibitors (TIMPs).
- Timely angiogenesis and neovascularization
- Low bacterial burden
|
- Chronic wounds fail to proceed through the normal phases of wound healing in an orderly or timely manner, often remaining in a stage of chronic inflammation
- Exudate contain high levels of MMP, suggesting slower tissue regeneration and delayed wound closure
- Prolonged inflammatory phase, impaired angiogenesis and neovascularization, resulting in insufficient oxygen and nutrient supply
- Biofilm formation and recurring infections
|
Partial vs. full-thickness wounds
Wound thickness can be classified as superficial, partial or full-thickness, as shown in Table 2.
- Superficial thickness wounds usually display an effective reorganization of the normal barrier function and anatomical structure of the skin, with complete healing.
- A wound may require cleaning or removal of debris and nonviable tissue for proper assessment of thickness.
Table 2. Wound thickness
| Wound thickness |
Description |
|
Superficial thickness

|
Extends from the epidermis to the most superficial portion of the dermis
|
|
Partial-thickness

|
Involves skin loss up to the lower dermis
|
|
Full-thickness

|
Involves skin and subcutaneous tissue
|
By etiology
Common wound causes are listed below:
- Acute burns
- Animal and insect bites
- Arterial insufficiency
- Auto-immune disorders
- Infectious ulcers
- Inflammatory ulcers
- Malignancy
- Mixed ulcers (arterial, venous, neuropathic, etc)
- Moisture-associated skin damage
- Neuropathy
- Pressure and shear
- Radiation injury
- Skin tears
- Surgery
- Trauma (abrasion, avulsion, laceration and perforation)
Types of wound closure
Wound closure can be classified as primary, secondary and delayed primary closure [17] :
Primary wound closure (or primary intention)
Wound closure may be achieved by approximating the wound margins with sutures using surgical stitches. This method, called wound closure by first (primary) intention, reduces the size of the wound and facilitates the process of wound healing.
Delayed primary wound closure (or tertiary intention)
Some more extensive wounds that cannot be closed primarily may be initially managed with local dressings and debridements, until the wound can be closed with interrupted sutures. This delayed method is referred to as healing by delayed primary wound closure or tertiary intention.
Secondary wound closure (or secondary intention)
When the decision is taken to achieve wound closure by physiological mechanisms of wound healing, through local debridement and application of dressings, wound closure is known as closure by second (or secondary) intention. The majority of chronic wounds that heal do so by secondary or tertiary intention.
THE WOUND HEALING PROCESS
Phases of normal wound healing
Wound healing is a vital event for the organism, to restore its cutaneous integrity. This process is made up of diverse mechanisms and complex signaling cascades which, when coordinated and synchronized, result in adequately healed tissue.[18] Didactically, the process of wound healing is divided into 4 overlapping stages (see Figure 3).
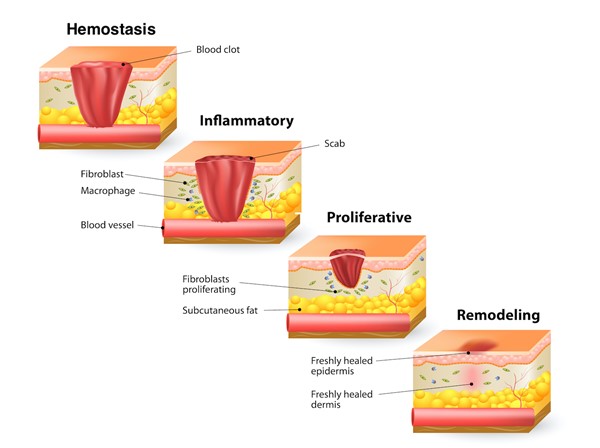
Fig. 3. Phases of wound healing
Hemostasis
When the skin is injured, hemostasis takes place in the next few minutes to control bleeding through the following mechanisms (Figure 4) [19] :
- Vasoconstriction: vasoconstriction reduces bleeding from injured vessels
- Fibrin clot formation: exposure of collagen type I activates proteases of the intrinsic and extrinsic pathways of coagulation. These activated proteases induce the conversion of prothrombin into thrombin, which in turn induces the conversion of fibrinogen into fibrin. Fibrin fibers come together to form a fibrin mesh which contains red blood cells and platelets, forming a clot at the site of the wound and blocking the flow from injured blood vessels.
-
Growth factor release and cell recruitment: the presence of the fibrin clot, red blood cells and platelets stimulates the release of growth factors, mainly by platelets. Notable among these are the Platelet-derived Growth Factor (PDGF), Transforming Growth Factor (TGF), basic Fibroblast Growth Factor (bFGF) and Vascular Endothelial Growth Factor (VEGF).These growth factors are chemotactic for fibroblasts, neutrophils and monocytes to the site of the wound. See section 'Appendix' below.
- Provisional matrix formation: in addition, another mechanism that helps in hemostasis is the formation of a provisional matrix from type III collagen which is synthesized by fibroblasts. This provisional matrix establishes a fluid environment that facilitates biochemical signaling.
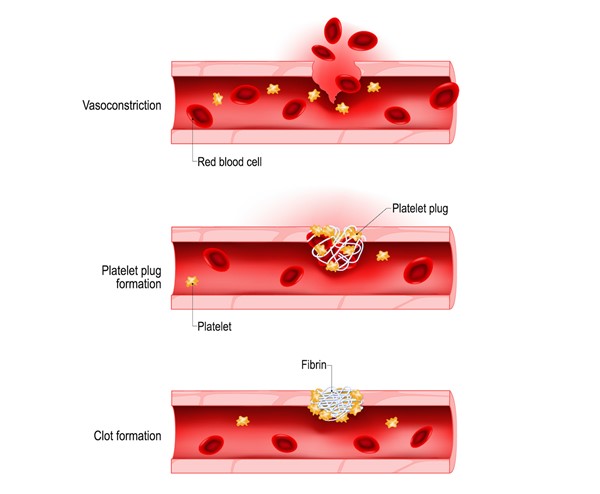
Fig. 4. Hemostasis
Inflammatory phase
As bleeding is stabilized, the next phase starts. The inflammatory phase usually lasts 2 weeks and is clinically characterized by tissue swelling, pain, redness and heat. Cutaneous injuries also stimulate the cutaneous neural system and trigger a cascade of events known as neurogenic inflammation. The inflammatory phase is characterized by:
-
Cell recruitment and activation: as the inflammatory phase progresses, more cells arrive in the injured site through diapedesis:
-
- Neutrophils are the first line of cellular defense and peak within 24-48 hours.
- Mastocytes continue their degranulation and release histamine, resulting in local vasodilation (manifested as redness of the wound), which facilitates diapedesis and plasma extravasation (manifested as perilesional edema). Edema facilitates biochemical cascades and actions of local mediators.
- This sequence of events activates and mediates the recruitment and activation of more neutrophils, eosinophils, lymphocytes, basophils and macrophages to the wound.
- T and B lymphocytes mediate humoral and cellular immune responses.
-
Neurogenic inflammation: which is characterized by release of vasoactive neuropeptides - predominantly Calcitonin Gene-related Peptide (CGRP), Substance P (SP) and Neurokinin A - by sensory nociceptive neural endings of the skin (neuron fibers type C and Aδ).[20]
-
- These neuropeptides lead to an inflammatory response cascade, including arteriolar vasodilation with extravasation of plasma proteins and degranulation of mastocytes in the injured tissue.
- Neuropeptides also stimulate keratinocytes, mastocytes, neutrophils and fibroblasts, resulting in pro-inflammatory positive feedback associated with growth, differentiation and immunomodulation at the wounded site.[21][22][23][24]
- Oxygen free radicals are released at the injured site.
- Matrix metalloproteinases (MMPs) are released in large quantities by neutrophils and activated macrophages. These proteases (mostly elastase and collagenase) remove damaged components of the extracellular matrix within the wound.
- In the final phase of inflammation, macrophages mediate the transition to the next stage of the repair process by releasing protease inhibitors, attenuating proteolytic destruction through the activity of PDGF, TGFβ and anti-inflammatory cytokines.
Proliferative phase
In this phase, which lasts approximately 24 days, fibroblasts are recruited more intensively, granulation tissue is produced and the wound decreases in size:
- Granulation tissue formation: within the wound matrix, which is rich in fibrin, fibroblasts multiply and synthesize collagen, fibronectin and proteoglycans. Simultaneously, white blood cells release TGFβ and VEGF, stimulating neo-angiogenesis. This combination gives rise to granulation tissue, which is basically composed of collagen and capillaries (Figure 5). This tissue serves as a transient substitute for the dermis.
-
Wound contraction: some fibroblasts differentiate into myofibroblasts.[25] Myofibroblasts are known for their capacity to produce new components of the extracellular matrix and for their ability to contract the wound. [26]
- Re-epithelialization: new epidermis is formed from the edges of the wound or from cutaneous appendages (Figure 5)
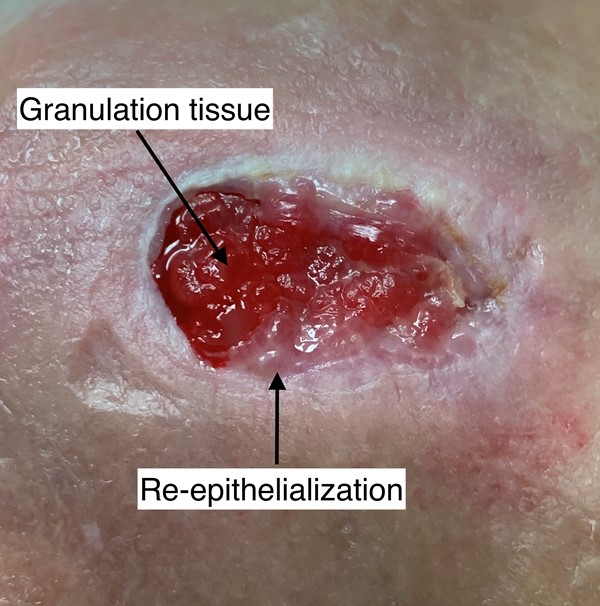
Fig. 5. Granulation tissue and re-epithelialization
Remodeling
The final phase of the process of wound healing - the remodeling phase - occurs over the first year after injury.
- Type III Collagen is replaced with type I Collagen. The organization and interlinking of collagen fibers increases the tensile strength of the scar tissue, which may reach nearly 80% of the tensile strength of the skin.
- The density of capillaries decreases, reducing the redness of the immature scar.
Regulation of wound healing by growth factors
Recruitment and activation of inflammatory cells during the wound healing process result from many signals provided by growth factors.[27] TGF-β is the most important growth factor during the wound healing process.[28] The TGF-β superfamily encompasses a diverse array of proteins, many of which play important roles during development, homeostasis, disease and repair of tissues, such as the skin. Other relevant growth factors include platelet-derived growth factors (PDGF), fibroblast growth factors (FGF), vascular endothelial growth factor (VEGF), etc. See section 'Appendix' below.
IMPAIRED WOUND HEALING
The process of wound healing can be compromised by local factors, systemic co-morbidities or both. Didactically, the process of wound healing may be “stalled”, for example in the inflammatory phase, thus perpetuating its chronic and deleterious state. Chronic wounds do not follow the normal course of cellular and molecular events which lead to a healthy wound closure.
Factors that may interfere with the process of normal wound healing are described below [2][29]:
- Accumulation of necrotic tissue;
- Altered profile of cytokines and increased inflammatory response;
- Co-morbidities (e.g. diabetes mellitus);
- Tobacco smoking (nicotine is a vasoconstrictor that reduces nutritional blood flow to the skin, resulting in tissue ischemia and impaired healing of injured tissue).[30]
- Alcoholism, illicit drugs
- Immobilization (mobility disorders) and tissue edema
- Inadequate and inappropriate interventions in wound care
- Increased enzymatic activity (proteases);
- Malnutrition (undernutrition and obesity);
- Older age
- Presence of biofilm, microorganisms, infection
- Stress (e.g. mechanical/ pressure and shear, psychological);
- The presence of free radicals (nitric oxide);
- Use of medications (e.g. corticosteroids, immunosuppressants)
The factors above influence the potential of the wound to heal, that is, its "healability". See "How to Determine Healability of a Chronic Wound".
Role of Biofilm
Biofilms are densely packed communities of microbial cells that grow on living or inert surfaces and surround themselves with secreted polymers.[31] Biofilm is present in most chronic wounds (Figure 6).[32] There is evidence that biofilm contributes to chronic inflammation in a wound.[33][34] Biofilms are not the cause of chronic wounds, but they can impede wound healing by impairing epithelialization and granulation tissue formation, and promoting a low-grade inflammatory response.[33][34]

Fig. 6. Chronic wound (left) and scanning electron micrograph of a Staphylococcus aureus biofilm (right)
-
Biofilm formation (Figure 7): Wounds provide an adequate habitat for bacteria, since loss of skin integrity provides a humid environment and availability of nutrients. The microbial population in deep tissues of chronic wounds is well-known and includes multiple bacteria species.[32] The majority of studies agree to the nearly universal presence of Staphylococcus aureus, but another common suspect encountered in chronic wounds is Pseudomonas aeruginosa, which in a study, was present in almost half of the wounds that were investigated.[32] When bacteria succeed in forming a biofilm structure on the wound bed, they become difficult to eradicate. The structure of the biofilm protects the bacteria from the activity of systemic and topical antibiotics, such as silver.[32]
-
Assessment of biofilm: the location, presence and slow growth of biofilms make it difficult to detect them by the naked eye or culture. For detection of biofilm in chronic wounds, The European Society for Clinical Microbiology and Infectious Diseases suggests taking a biopsy from the base of the debrided wound, as opposed to collecting swabs.[35] Swabs may yield false results due to contamination from the skin flora, strong adherence of biofilm to the host epithelium and growth of anaerobes in deep tissues. If soft tissue biopsy cannot be obtained, a superficial swab may be used to guide choice of antibiotic therapy.[35] More recent techniques include use of a point-of-care fluorescence imaging for real-time detection of porphyrin-producing wound bacteria.[36]
- Prevention and management: an effective approach to managing biofilms would be to avoid the formation of biofilm by interfering with the mechanisms of microbial fixation or with the processes involved in its maturation. Another way would be to remove or break up the mature biofilm in a mechanical manner (debridement). As of today, no strategy has been demonstrated to be completely effective against biofilm formation. Even so, combinations of various strategies, using systemic and topical medications, in association with debridement, have been used to fight against biofilm.
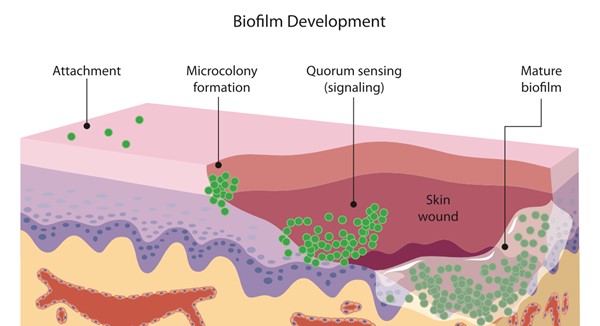
Fig. 7. Biofilm development.[37] Planktonic bacteria (e.g. Staphylococci, Streptococci, Pseudomonas) attach to the skin surface. Once attached, microbes form microcolonies within 2-4 hours. Bacterial cells communicate with each through signals (quorum sensing), which controls biofilm formation in many bacterial species.[38][39] Bacteria secrete a protective surrounding matrix known as extracellular polymeric substance (EPS) and, as a result, the micro-colonies become increasingly tolerant to biocides (mature biofilm).
PATHOLOGICAL SCARRING
The word scar originated primarily from the Greek language with the word eschara, which means "home". The eschara was situated in the center of the house, and around it all domestic life would take place. Because of these activities, and because of the gathering of children and domestic workers around the fire, burns used to be so frequent that the name of the cause became synonymous with the effect (eschar). In ancient Rome the word eschara became cicatrix. Subsequently, in France it was translated to eschare, and in Britain in scaur. In the Middle Ages the word cicatrix obtained several meanings, covering any white spot on the skin, including scleroderma, morphea, vitiligo and even leukonychia.[40]
Types of scar
Scars can be classified as normotrophic or pathological [41]:
- Normotrophic: scars that result from normal a wound healing process
- Pathological: abnormal scarring, which can be subclassified as atrophic and fibroproliferative:
-
- Atrophic: an example is striae distensae
- Fibroproliferative: such as keloid and hypertrophic scar
Scars also may be hypo, normo or hyperpigmented. However, in clinical practice, scars appear in a mixed form, that is, with one or more combinations of the types above mentioned.[42][43]
Atrophic scars
The main pathological characteristic of atrophic scars is the loss of elasticity and their histological architecture. Most commonly, the epidermal layer becomes atrophic. Dermal atrophy would imply a more serious cutaneous lesion. Still, when the subcutaneous tissue is also compromised, these scars are called panatrophic.[41][44]
- Epidermal atrophy: examples of scars with epidermal atrophy and rectification of the dermo-epidermal papillae include post-vaccinal scars, healed shingles, cutaneous abrasions and superficial second degree burns (Figure 8A).
- Dermal atrophy: the most common examples are stretch marks (striae distensae) and acne (boxcar, icepick and rolling) (Figure 8B). Dermal atrophy is more common among teenagers, and is frequently seen in the mammary region, abdominal wall, thighs and arms. In this age group, increased secretion of glucocorticoids decreases collagen synthesis and number of mast cells at the scar site, and increases collagenase activity, predisposing to cicatricial atrophy.
- Panatrophy: examples include scars resulting from deep burns, external fixators and subcutaneous abscesses (Figure 8C).
Atrophic scars have also been considered a variation of normotrophic scars, by modification of the maturation phase of wound healing due to location, mobility and tension of the scar. Ethnic factors are not thought to predispose an individual to the development of atrophic scars.
|

Fig. 8A. Atrophic epidermal scar due to vaccine
|
 Fig. 8B. Atrophic and enlarged dermal scar post abdominal surgery Fig. 8B. Atrophic and enlarged dermal scar post abdominal surgery
|
 Fig. 8C. Panatrophic scars on lower right limb due to chronic use of orthopedic external fixators Fig. 8C. Panatrophic scars on lower right limb due to chronic use of orthopedic external fixators
|
Fibroproliferative scars (keloid and hypertrophic scar)
Hypertrophic scars and keloids result from abnormalities in the physiological process of wound healing. These fibroproliferative diseases of the skin present a great therapeutic dilemma and challenge to clinicians, as they are disfiguring and frequently recur after surgical resection.
- Clinical characteristics of fibroproliferative scars include:
-
- Keloid: pathological scars that spread into the surrounding normal skin (Figure 9A)
- Hypertrophic scar: pathological scars that do not grow beyond the boundaries of the original wound (Figure 9B)
-
Pathophysiology: it has been postulated that hypertrophic scars and keloids are actually manifestations of the same fibroproliferative skin disorder, but with different intensity and duration of inflammation.[45] Pathological scars are characterized by continuous local inflammation. This scenario contributes to an increase in inflammatory infiltration, in fibroblast numbers, in neovascularization and in deposition of collagen in the reticular dermis. It is thought that the intensity, frequency and duration of inflammatory stimuli (exogenous and endogenous) determine the activity, direction, growth rate and exuberance of related clinical symptoms.[21][43][45] Wound healing is a physiological event and, therefore, it is also subject to the influences of the nervous, endocrine and immune system, as well as of emotions.[21][46] Hypertrophic scars and keloids have a greater number of nerve fibers compared to mature scars and the skin itself.[47] This characteristic, in theory, could be responsible for the development of fibroproliferative scars, as there is evidence that cutaneous innervation plays an important role in mediating normal wound healing (although it is not known if the higher concentration of nerve endings is present before the cutaneous lesion, or if more nerve endings develop after the wound has started to heal).
-
- Several neuropeptides and neurotransmitters secreted by sensory and autonomic nerve fibers play essential roles during the different phases of wound healing. Neurogenic inflammation and growth factors activate fibroblasts in their proliferative activities (i.e., collagen production).
- NGF induces release of neuropeptides by sensory fibers, leading to accumulation of neuropeptides in the cutaneous tissue, and a vicious cycle of inflammation. [21][45] See section 'The Wound Healing Process - Inflammatory Phase‘ above.
- Abnormal wound healing should be interpreted holistically, from a psychoneuroimmunendocrine functional perspective.[48] Wound healing depends on neurogenic factors (electrical and neurosecretory) that, in turn, are modulated by psychological aspects and adjusted by immunological and endocrine factors. Any changes in these systems could interfere in the normal progress of a scar tissue formation, resulting in deficit in atrophic scars and hyperproliferative scarring in hypertrophic scars and keloid.
|
 Fig. 9A. Keloids on the anterior thoracic region of endogenous injury origin (acne) Fig. 9A. Keloids on the anterior thoracic region of endogenous injury origin (acne)
|
 Fig. 9B. Hypertrophic scar on the anterior thorax after surgical procedure (exogenous injury origin). Fig. 9B. Hypertrophic scar on the anterior thorax after surgical procedure (exogenous injury origin).
|
APPENDIX
Growth factors in wound healing
TGF-β is the most important growth factor during the wound healing process.[28] The TGF-β superfamily encompasses a diverse array of proteins, many of which play important roles during development, homeostasis, disease and repair of tissues, such as the skin.[49] TGF-β and other growth factors present at the wound site are described in Table 3 below. There are other families and subtypes of growth factors whose functions and interactions are important in all the complexity of the wound healing process.
Table 3. Partial list of growth factors present at the wound site
TGF-β: transforming growth factor beta, PDGF: platelet-derived growth factor, FGF: fibroblast growth factor, VEGF: vascular endothelial cell growth factor, NGF: neural growth factor
| Growth Factor |
Biologic Activity |
TGF-β
|
- TGF-β stimulates the expression of extracellular matrix proteins and integrins. There are three isoforms of TGF-β (TGF-β1, β2 and β3)
-
- Immediately after injury, TGF-β1 is released from platelets, serving as a chemoattractant for neutrophils, macrophages and fibroblasts at the site of the injury. On the basis of the pattern of the expression of TGF-β and its receptors in the cutaneous wound, it has been suggested that it stimulates re-epithelialization and the formation of granulation tissue. In addition, by inducing integrins, TGF-β promotes the migration of keratinocytes through the provisional wound matrix. TGF-β stimulates angiogenesis, proliferation of fibroblasts, differentiation of myofibroblasts and deposition of matrix.
|
PDGF
|
- PDGF was the first growth factor to be identified as having a chemotactic function, attracting neutrophils, monocytes and fibroblasts. Furthermore, PDGF increases proliferation of fibroblasts and production of extracellular matrix by these cells. Finally, it stimulates fibroblasts to contract the collagen matrix and induces their differentiation into myofibroblasts.[49]
|
FGF
|
- FGF are a family of polypeptide growth factors made up of 22 types. The majority of these types have a broad mitogenic spectrum. They stimulate the proliferation of various cells of mesodermal, ectodermal and endodermal origin. The only exception is FGF7 (Keratinocyte Growth Factor, KGF), which is more specific to epithelial cells, at least in the adult body. Apart from these mitogenic effects, FGFs also regulate the migration and differentiation of their target cells, and some FGFs demonstrate cytoprotective activities. The expression of FGF1, FGF2, FGF5 and FGF7 was found in the skin and in wounds, and the expression of all these FGFs increased after skin lesions. It has been suggested that FGF7 stimulates wound re-epithelialization in a paracrine manner. [49]
|
| VEGF |
- VEGF family currently includes VEGF-A, VEGF-B, VEGF-C, VEGF-D, VEGF-E and Placenta-derived Growth Factor (PLGF). [49]
-
- VEGF-A was identified as an important regulator of angiogenesis during wound healing.
|
| NGF |
- NGF is a prototype of the neurotrophin family, which is essential for the development and survival of central and peripheral neurons. Furthermore, it plays a fundamental role in triggering and maintaining inflammation in various organs, such as in the repair of cutaneous wounds. In addition, the levels of NGF also increase at injured sites, in recently-formed epithelial cells at the margins of the wound and in fibroblasts of the granulation tissue. [49]
|
Official reprint from WoundReference® woundreference.com ©2026 Wound Reference, Inc. All Rights Reserved
NOTE: This is a controlled document. This document is not a substitute for proper training, experience, and exercising of professional judgment. While every effort has been made to ensure the accuracy of the contents, neither the authors nor the Wound Reference, Inc. give any guarantee as to the accuracy of the information contained in them nor accept any liability, with respect to loss, damage, injury or expense arising from any such errors or omissions in the contents of the work.