ABSTRACT
This topic provides practical guidance to wound care clinicians on the selection of Negative Pressure Wound Therapy (NPWT) devices, device application, and assessment of therapy effectiveness. For background information on NPWT including indications and contraindications, see "Negative Pressure Wound Therapy". For decision support on different brands of both disposable and durable NPWT devices and dressings, see NPWT Interactive Matrices for "NPWT Disposable Pumps", "NPWT Durable Pumps" and "NPWT Dressings". To assess if NPWT is indicated for a specific wound type, use the Wound Prep & Dress Tool. For a case series of circumferential NPWT, see "Case: Circumferential Negative Pressure Wound Therapy".
Practice Tips are summarized below. For detailed description, rationale and pictures on use of NPWT with or without application of cleansing solution, see section 'How to Apply' on this topic. For guidance on clinical effectiveness and criteria for continued benefit coverage, see section 'How to Assess Effectiveness'. For a systematic assessment of malfunctioning alarms and potential solutions, see section 'Troubleshooting'.
Do:
- Review safety information and instructional manual for the specific NPWT system before application.
- Confirm order for NPWT is present, including settings, dressing type, and frequency.
- Ensure patient is medicated for pain prior to application.
- Remove all pieces of previous dressing.
- Perform thorough wound assessment, noting any exposed structures that may need protection or nonviable tissue that may need debridement.
- Cleanse wound and apply any desired barriers to periwound.
- Apply selected dressing medium, ensuring complete contact with wound bed, and cover with adhesive film dressing.
- Cut generous opening in adhesive film dressing and apply suction tubing and ensure canister is engaged in device before initiating therapy.
Don’t:
- Apply NPWT without specific orders.
- Leave any material in wound bed unless specifically directed by prescribing provider (grafts, suture material, etc).
- Apply NPWT over gross necrosis or insert foam into unexplored tunnels or sinus tracts.
- Cut linear opening in in adhesive film to attach suction tubing, this may seal closed and occlude therapy
- Cut dressing too thin, as it may not conduct and appropriately evacuate exudate.
- Pack foam tightly into wound, this can cause tissue ischemia and/or act as a physical barrier to granulation tissue formation.
- Stretch the adhesive film dressing; this can cause epidermal trauma or blistering to the periwound.
For assessment NPWT effectiveness, see section 'How to Assess Effectiveness' on this topic.
Video 1. Application of traditional NPWT | Video 2. Troubleshooting: traditional NPWT
|
HOW TO SELECT AN APPROPRIATE DEVICE
NPWT may be delivered through an array of devices with varying features. Device selection may be guided by relevant questions such as the ones below:
- For what primary indication will the NPWT device be used?
-
- Most NPWT units carry similar indications, spanning from chronic wounds failing traditional therapies to acute and surgically created wounds. Specific NPWTs limited to single indications include incisional NPWT for primarily closed surgical incisions, and open abdomen therapy (e.g, AbThera, Acelity) for conditions requiring delayed, staged closure of the abdomen including abdominal compartment syndrome and others. For select patients, including those with substantial comorbidities that are known to impair wound healing and/or response to infection (e.g., complex hosts), or those who have a clinically complex wound, NPWT with application of cleansing solution may be used.[1] See indications for each type of NPWT device in the section 'General Indications and Contraindications' in topic "Negative Pressure Wound Therapy".
- Negative pressure settings: pressure settings vary according to indication. Devices differ with respect to range of pressure settings offered, but typically run in 25mmHg increments from -25mmHg to -200mmHg, and may offer both continuous and varied negative pressure options.
- How much exudate does the wound have?
-
- Exudate collection system: most NPWT devices utilize a closed canister collection system with varying capacities for wound exudate, and some systems offer multiple canister sizes. While most devices have external, replaceable canisters, some will have internal collection canisters, or simply trap exudate inside the dressing.
- What are the characteristics of the wound?
-
- Dressing medium: most dressings can be used alone or in combination depending on the wound environment and presence of structures, tunneling, or other material present such as grafts (e.g. more dense foams for tunneling as to decrease likelihood of tearing during removal or to create less tissue ingrowth over fragile structures, or gauze composite dressings for more superficial ulcerations). Dressings are specific to each NPWT device, and most are composed of foams (polyurethane, polyvinyl alcohol, etc), hydrocolloids, gauze, and some textiles. Some manufacturers offer multiple varieties of dressings including antimicrobial options.
- In which setting is the patient being treated (inpatient vs. outpatient)? Is there a need for mobility?
-
- Power source: will differ based on whether the device is reuseable (durable) or disposable. Durable units are maintained after each use, and re-used for multiple patients, while disposable devices are discarded after use on one patient, and not maintained and re-used. Durable devices are electrically powered and have an internal battery which can be recharged hundreds of times with an AC adapter plugged in to electricity via wall outlet; they typically have a battery life of several hours or more. Disposable devices may also have an internal battery, but with limited recharge capability (e.g. 7-14 days), and may come with an AC adapter to charge via wall outlet. Some disposable devices are not electrically powered and do not contain a battery or require recharging via wall outlet.
- Use of wound bed cleansing solutions: NPWT with cleansing solutions is currently utilized only in inpatient settings.
- Portability: some NPWT devices are designed to be carried as a shoulder bag, and some devices can be worn under clothes allowing mobility for patients who need it, or allowing for concealment of the device.
- How often will personnel be available to change NPWT dressings?
-
- Frequency of NPWT dressing change: frequency depends on manufacturer recommendations for device and specific dressing type utilized, patient condition, wound severity, exudate levels, need for re-evaluation of wound bed, etc, but most NPWT dressings will be changed 2-3 times weekly. Incisional NPT or other smaller disposable systems may be left in place for 7-14 days.
- What are the coverage/reimbursement criteria observed by the patient's insurance?
-
-
Device acquisition/reimbursement mechanism: Medicare and private insurers have different coverage policies depending on factors such as types of NPWT devices and supplies, and setting where it is being used (e.g., outpatient, inpatient, etc). For coding, coverage and reimbursement information, see Section on 'Coding, Coverage and Reimbursement' in "Negative Pressure Wound Therapy".
HOW TO APPLY A NPWT DEVICE
Steps and Rationale
Traditional NPWT
The table below illustrates general guidelines for application of traditional NPWT devices on wounds. Please refer to manufacturers' literature for specific instructions
| Steps |
Rationale/ Tips |
|
1. Please review safety information and instructional manual for the specific NPWT system before application.
|
- Be aware of your resources, set up an inservice from the product representative and keep their contact information handy.
- Be familiar with the product indications, contraindications, and compatible therapies).
|
|
2. Confirm there is an order for device settings and dressing change frequency.
|
- Having this information beforehand can avoid confusion and interruptions in therapy
|
3. Ensure patient is adequately medicated for pain prior to dressing application or change.
|
- For removal of dressings, please consider hydration of the dressing with saline, wound cleanser, or topical anesthetic agent to reduce patient discomfort during dressing change. Therapy can also be powered off for 10-20 minutes prior to assist with separation of dressing from the wound bed.
|
4. Remove previous dressing if applicable, ensuring all pieces of foam or gauze are removed. Dispose per organizational policy.
|
- If possible, educate staff and create a system where all clinicians routinely document the number of dressing pieces applied to the wound bed
|
5. Non-viable tissue should be debrided as needed
|
- Wound healing will take place more rapidly if the wound is free of /debris and devitalized tissue; mechanical debridement can be performed as needed during dressing changes to remove sessile tissue, but more invasive excisional debridement may need to be performed for more adherent slough or eschar
|
6. Cleanse wound and periwound per orders or organizational protocol.
|
- Ensure cleansing agent utilized is proven non-cytotoxic to healthy tissue
|
7. Use skin protectant or barrier as desired prior to applying adhesive film dressing, ensuring skin is clean and dry prior to application.
|
- Intact periwound skin will be more likely to remain in good condition and risk of skin complications such as contact dermatitis can be decreased, and broken periwound skin will improve more readily and decrease likelihood of superimposed fungal or bacterial infection if appropriate steps are taken to apply barriers before application of adhesive drapes
|
8. Assess wound for:
- Adequate hemostasis
- Exposed structures or sharp bony edges—do not apply over vessels or bowel, use nonadherent porous or fenestrated dressing that will transfer exudate when placed over structures such as tendon or bone for protection
- Unexplored tunneling—do not place dressings into these areas
|
- Attention to assessment of these factors will prevent adverse effects such as uncontrolled bleeding, tissue injury related to sharp bony edges, or untoward effects such as fistulization or injury of other structures in unexplored tunnels
|
9. After application of skin barrier to periwound, allow skin to dry, apply adhesive film dressing (commonly done in strips), unless otherwise recommended by manufacturer
|
- Pre-draping the periwound skin prior to dressing application is not always required, but can be helpful in some areas where cutting the dressing to exact dimensions is not efficient or feasible.
- Pre-draping allows for some overlap of foam onto the periwound without tissue damage.
|
10. Cut foam to fit dimensions or select appropriate sized gauze dressing, ensuring contact with tunneling or undermining if present without tightly packing or allowing dressing medium to contact intact skin edges. See Video 1 below.
|
- Ensure debris from cut dressing do not fall into wound bed, these can cause foreign body reaction or act as nidus for infection.
- If multiple pieces of dressing medium are used, write this information on the adhesive film dressing as to avoid retained material.
- Any other additional products may be added to the wound bed at this time in accordance with specific device specifications/indications for use (e.g. if wound requires contact layer for protection of structures or additional dressing mediums for varying tissue qualities such as moist gauze or foam for friable tissue). Understand that different topical mediums may affect the negative pressure conduction to the wound bed, sometimes adversely. Ensure benefit outweighs risk.
- Do not overpack wound.
- For use of NPWT on skin grafts, apply a non-adherent layer on the skin graft first [e.g. fenestrated silicon contact layer (e.g. Mepitel One), gauze impregnated with paraffin] followed by open cell polyurethane foam (cut to fit the contour of the wound).[2][3]
|
11. Place adhesive film dressing in a manner covering the entire surface of the dressing medium with a generous margin onto surrounding healthy periwound tissue, approximately 5cm or more if needed. Do not stretch adhesive film dressing, as this can cause shearing or blister formation on the skin.
|
- If difficult anatomy or area of high moisture is involved, or minimal healthy periwound margin is available, products such as ostomy rings, strips, or paste can be utilized.

|
12. Choose suction pad site, understanding that in ambulatory patients, the tubing may need to be pointed in a specific direction for best functionality. An example would be a lower extremity wound with the suction tubing pointed upward so it can run upward through the patient’s pant leg.
|
- If suction tubing may cause excessive pressure on underlying skin, create a bridge with a layer of adhesive film dressing, dressing medium, and additional adhesive drape under and over dressing, to conduct suction to another location which will not cause excessive pressure. An example would be a coccygeal wound, where a bridge of dressing medium would need to be placed to the lateral side of the trunk, hip, or thigh.

|
13. Cut appropriately sized hole in adhesive film dressing and apply suction pad. The dressing medium does not need to be cut and removed during this step.
|
- Do not cut a single slit in adhesive film dressing, as this may seal on itself during initiation of therapy and occlude conduction of negative pressure and flow of exudate.
- Make a dime to nickel size opening. Recommendations vary per manufacturer and range from 1cm to quarter-sized opening.
|
14. Power on NPWT unit and install exudate collection container (for powered units). For non powered units, follow instructions to charge suction chamber.
|
- Ensure there is an adequate supply of dressings and exudate collection containers available, both for future dressing changes and to replace one that may be contaminated or does not function appropriately
- Pressure settings vary according to indication and range from -25mmHg to -200mmHg, with -175mmHg being one of the most common
- For use of NPWT on skin grafts, pressure at -80 mmHg is recommended in order to promote graft take.[4]
- For use of NPWT on cellular and/or tissue based products (CTP), a negative pressure level up to -125 mmHg, and intermittent vacuum suction have been suggested.[5] See topic "Negative Pressure Wound Therapy".
|
15. Connect tubing from exudate collection container to suction tubing and ensure any clamps are open.
|
- Tubing can be secured over a layer of padding on adjacent intact skin by using additional adhesive film dressing, gauze and tape, or other securement to allow for maximum patient mobility and decrease risk of accidental tube dislodgement.
|
16. Troubleshoot any leaks as needed.
|
- Leaks can be prevented with adequate skin preparation and barrier application, and further addressed with additional application of adhesive film, ostomy products such as rings, strips, or paste.
|
17. Repeat steps for dressing change/reapplication.
|
- See “How to Assess Therapy Effectiveness” below
|
Video 1. Application of traditional NPWT
Video 1. Application of NPWT on a dehisced surgical wound on the chest, status post removal of infected pacemaker. By S. Robinson, M.D.
NPWT with application of cleansing solution
Once NPWT with application of cleansing solution is indicated, an expert consensus recommends that clinicians [6]:
- Identify goals of care (e.g. wound cleansing/reduction of bioburden, removal of devitalized tissue),
- Start a 2-week challenge with NPWT with instillation therapy
- Monitor progress against goals of care at week 1, and
- Reassess progress against goals of care at the end of week 2 of therapy and decide next step (e.g. continue to full granulation/surface level epithelization if possible, prepare for definitive reconstruction, stop or change therapy if objectives not met).
Many of the techniques illustrated on the table above for traditional NPWT can be used for NPWT with application of cleansing solution. Please refer to manufacturers' literature for specific instructions. Settings and cleansing solution vary, most experts agree on the following [7][8]:
- Settings: 10-20 minutes of soaking time, -125 mmHg of negative pressure, with 1-4 hours of vacuum time,
- Cleansing solution: cleansing with normal saline, acetic acid, or hypochlorous acid.
Other tips include:
- Bridging wounds: place the solution delivery pad in the less dependent wound/area. In that way, gravity will help filling the foam of the lowest (more dependent) wound.
- Determining the amount of solution: take into account wound depth (less solution for shallow wounds), number of wounds (bridged wounds require more solution to fill all wounds), presence of undermining (extra fluid is required)
- Minimizing leaks: select adequate volume of solution to avoid overfilling, minimize patient's activity during application of cleansing solution, use stoma paste and/or hydrocolloid dressing to achieve good seal in crevices, cracks or wet areas.
NPWT on Trochanteric Ulcer

Figure 1a. Trochanteric pressure ulcer stage IV | 
Figure 1b. Draping periwound |

Figure 1c. Draping completed | 
Figure 1d. Applying nonadherent antimicrobial layer (Acticoat Flex 3) |

Figure 1e. Foam applied and draped over | 
Figure 1f. Opening for suction tubing |

Figure 1g. Tubing applied | 
Figure 1h. Suction on and dressing vacuum at skin level |
NPWT on Lower Limb Ulcer

Figure 2a. Lower limb ulcer of traumatic etiology | 
Figure 2b. Assessing undermining |

Figure 2c. Periwound draping | 
Figure 2d. Applying foam and draping over |

Figure 2e. Opening for suction tubing | 
Figure 2f. Tubing attached |

Figure 2g. Suction on -125 mmHg continuous |
|
HOW TO ASSESS EFFECTIVENESS OF NPWT
Systems have varying indications and differ with advertised functionality. Some systems are suited principally for exudate management, whereas others may decrease bioburden and promote wound contraction. Depending on the NPWT system, performing thorough serial wound assessments may reveal decrease in wound dimensions, increase in granulation tissue, decrease in presence of nonviable tissue, decrease in periwound and surrounding tissue edema, decrease in periwound maceration, among others. Units covered under the DME benefit of insurance plans may require demonstrable evidence of decreased wound dimensions for continued therapy and coverage of the device.
If any measurable degree of wound healing has failed to occur over the prior month, clinicians may consider discontinuing NPWT and reassessing the plan of care, as recommended by Noridian Medicare Local Coverage Determination.[9] Wound healing is defined as improvement occurring in either surface area (length times width) or depth of the wound (Figures 3a-3d) It should be noted that a decrease in wound depth alone may not be considered sufficient progress with respect to continued insurance approval for NPWT DME products.
 Figure 3a. Large mass and abscess on the neck, pre surgical excision. Pathology report indicated abscess and ulcer with focal atypical squamous proliferation, but low probability of neoplasia. Figure 3a. Large mass and abscess on the neck, pre surgical excision. Pathology report indicated abscess and ulcer with focal atypical squamous proliferation, but low probability of neoplasia.
|  Figure 3b. Left: Neck defect, immediately after surgical excision of the mass. Right: Appearance of the wound 2 weeks after initiating NPWT with application of cleansing solution, and foam interface (note that the interface has a contact layer with round through holes). Figure 3b. Left: Neck defect, immediately after surgical excision of the mass. Right: Appearance of the wound 2 weeks after initiating NPWT with application of cleansing solution, and foam interface (note that the interface has a contact layer with round through holes).
|
 Figure 3c. Signs of improvement of the wound with decrease in wound dimensions and depth. Picture taken after 4 weeks of NPWT (two weeks of NPWT with application of cleansing solution, followed by 2 weeks of NPWT without cleansing solution) Figure 3c. Signs of improvement of the wound with decrease in wound dimensions and depth. Picture taken after 4 weeks of NPWT (two weeks of NPWT with application of cleansing solution, followed by 2 weeks of NPWT without cleansing solution)
|

Figure 3d. 13 days post-op split thickness skin grafting (STSG) with 100% take, performed 10 days after image in figure 3c.
|
WHEN TO DISCONTINUE NPWT
Cessation of NPWT is recommended when [10]:
- Wound bed is covered by healthy granulation
- There is evidence of necrotic tissue, hypergranulation, or stagnation
- If the wound does not show adequate signs of healing within 2 weeks of NPWT
- Use of NPWT is not appropriate (e.g., negative pressure is difficult to maintain because of the location of the wound)
- Healthcare professionals authorized to change the dressings are lacking
- Moderately severe adverse events occur, namely:
- Excessive bleeding
- Severe wound or periwound infection
- Intense pain
- Allergic reaction following application
- Patients and/or their caregivers do not adhere to the treatment
TROUBLESHOOTING
Opportunities for misapplication of NPWT are numerous. Even if there are designated clinicians in charge of application of NPWT, it is important that all staff, particularly nursing, have regular training and competency updates to troubleshoot alarms, repair leaks and observe for complications.[11] An assessment method, common alarms and potential causes and solutions are presented below.
Systematic Assessment
Always assess alarms in a systematic manner, as follows (Figure 4):
- Start with the machine, ensuring canister is engaged appropriately without cracks (do NOT slam canister into place to engage it, as this can create micro cracks in the plastic and cause leaks),
- Inspect tubing connectors,
- Inspect the tubing clamps,
- Inspect the suction pad,
- Inspect the drape covering the wound.
Occasionally, the machine is the culprit and has malfunctioned. Typically, if the machine side tubing is clamped and a leak alarm is still present, there is a canister or machine problem. If both canister and machine issues are ruled out or resolved, and this does not stop the alarm, the issue could be the patient side tubing or the dressing itself.
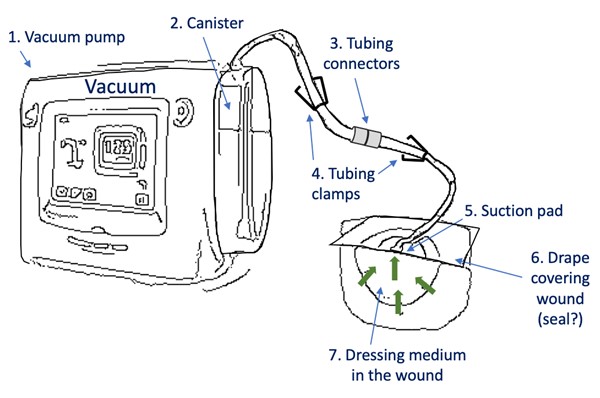
Figure 4. Systematic assessment of NPWT alarms (sample schematic of one of the most common configurations, configurations may vary)
Common Issues - Traditional NPWT
Common alarms
Common alarms are due to blockage, leak, canister full, canister not engaged, therapy inactive, low pressure, battery low/critical, temperature alert, pressure deviation.[12][13] Always consult the manufacturer's troubleshooting guide for specific recommendations.
Most common causes of blockage alarm
- Hole cut in drape for suction pad too small
- Suction pad is over drape or skin instead of foam
- Suction pad is folded or compressed in contour of wound
- Clamps on patient side or machine side tubing closed
- Exudate too thick
- Tubing is kinked or compressed/crushed
- Foam between wound bed and suction pad is too thin, causing collapse of foam
- Unit and tubing are elevated higher than wound site (drop unit and tubing below level of wound)
- Patient position is causing any of the above issues temporarily
Most common causes of leak alarm:
- Drape “wrinkle” extending from foam to edge of drape
- Tubing incompletely connected to machine
- Canister not fully engaged
- Crack in canister
- Canister seals missing (where canister connects to unit)
- For some units, the wound may be too large for the unit's vacuum power and is unable sufficiently hold seal at set parameters
- Faulty suction pad/tubing
- Highly exuding wounds can cause a leak in the drape seal prior to engaging unit and beginning therapy
Common causes of skin irritation:
- Inadequate periwound preparation/ protection
- Stretch applied to the occlusive drape during application
- Excessive layers of drape
- Foam overlapping onto intact skin during dressing application, or as a result of interruption in therapy which allowed foam to shift while therapy was inactive
Common NPWT-related causes of lack of wound healing progress
- Pressure too low or too high
- Too much foam placed in wound (overpacking)
- Foam isn’t “combed” prior to placing in wound, creating inflammation and foreign body-type reactions from retained foam
- Wound has become too dry for NPWT and is further desiccated by the NPWT
- Wound has become infected
Video 2. Troubleshooting traditional NPWT
Video 2. Troubleshooting traditional NPWT. By Amanda Burkeybile LPN, CWCA and Rachel Kinney RN, CHRN
Common Issues - NPWT with application of cleansing solution
Common alarms
Common alarms are due to lack of solution, solution tubing blockage, solution canister not engaged, blockage and leak. Always consult the manufacturer's troubleshooting guide for specific recommendations.
Most common causes of blockage alarm
- Tissue loosened by fluid movement has occluded the suction pad
- Cleansing solution has precipitated and occluded the suction pad
- Cleansing solution tubing kinked
- Hole cut for cleansing solution pad not large enough
Most common causes of leak alarm
- Inadequate skin prep and periwound sealing with adjunctive tools/dressings
- Too much cleansing solution being applied
- Excessive patient movement during soak time
- Dressing not changed with appropriate frequency, compromising integrity of drape and sealing agents secondary to frequent presence of cleansing solution
REVISION UPDATES
| Date | Comments |
| 3/2/25 | Added sections on application of NPWT on skin grafts |
| 4/8/22 | Version 2. Added videos on how to apply traditional NPWT and troubleshooting traditional NPWT
|
Topics are updated as new evidence arises. Major updates are noted above.