ABSTRACT
According to the International Skin Tear Advisory Panel (ISTAP), the updated definition of a skin tear (ST) is as follows: "Skin tear is a traumatic wound caused by mechanical forces, including removal of adhesives. Severity may vary by depth (not extending through the subcutaneous layer).”[1] The incidence of STs among elderly people living in long-term care facilities has been reported to range between 2.23 to 92%.[2][3] This topic provides a review and framework for assessment of patients with STs (e.g. epidemiology, risk factors, etiology, pathophysiology, history, physical examination, diagnosis, differential diagnoses, documentation and ICD-10 coding).
For a clinical pathway on ST assessment for use at the point-of-care, see 'Algorithm for Assessment of Skin Tears' (includes risk assessment algorithm)
Risk factors: The ISTAP groups risk factors in 3 categories [4]: general health (e.g. chronic and critical disease, polypharmacy), mobility (e.g. history of falls, impaired mobility), and skin (e.g. fragile skin, extremes of age). The most prevalent risk factors for STs are old age, impaired mobility, falls and accidental injuries, previous STs, cognitive deficit/dementia, dependence in transfers, and STs in upper limbs.[3]
History: Patients with STs need a comprehensive history including risk assessment, chief complaint/history of present illness, medications, social history, review of systems, nutritional assessment, patient's/caregiver's concerns.
Physical examination: Patients with ST should be thoroughly examined. Focused examination includes skin/integument and wound assessment. STs occur mainly on the upper and lower limbs of elderly persons. They may have a skin flap (i.e. a portion of the skin that is unintentionally separated from its original place due to shear, friction and/or blunt force).
Diagnosis: Diagnosis is clinical, based on history and physical examination.
Differential diagnoses: Include Stage 2 pressure ulcers/injuries, deep tissue injuries, moisture-associated dermatitis, tape burns, hematoma. See topic "Pressure Ulcers/Injuries - Is it Really a Stage 2?"
Classification systems: the ISTAP classification is the most utilized (type 1: no skin tear; type 2: partial flap loss; type 3: total flap loss)
Ulcer prognosis (healability) assessment: Aims to determine whether the ulcer can be healed with active conservative management alone (healable) or not (non-healable) or if co-existing medical conditions, drugs or circumstances will likely impede wound healing (maintenance). Determination of ulcer healability helps creation of an adequate treatment plan.
Documentation: Proper documentation should be completed upon first assessment and least once a week and more often as needed; adequate documentation helps track wound healing progress. Signs of ulcer improvement need to be documented to support medical necessity (as per Medicare requirements).
Coding: see guidance for ICD-10 coding, Medicare MDS (long-term care facilities), Medicare OASIS-D (home health agencies)
Treatment: See topic " Skin Tears - Treatment and Prevention"
When to refer to specialists:
- Wound specialist if ST does not show signs of improvement in 7-21 days.
- Registered dietitian if at risk for malnutrition
- Respective specialists if associated metabolic, hematologic, autoimmune, oncologic diseases are suspected.
- Social work for economic and social support.
- Psychologist/ mental health professional for depression and other psychological issues.
Algorithm for Assessment of Skin Tears |
INTRODUCTION
Overview
This topic provides a review on Skin Tears (ST) and framework for ST assessment. It includes epidemiology, risk factors, etiology, pathophysiology, history, physical examination, diagnosis, differential diagnoses, documentation and ICD-10 coding. For treatment and prevention of STs, see topic "Skin Tears - Treatment and Prevention".
Background
Definition
- The updated definition of a skin tear (ST) by the International Skin Tear Advisory Panel (ISTAP) is as follows: "Skin tear is a traumatic wound caused by mechanical forces, including removal of adhesives. Severity may vary by depth (not extending through the subcutaneous layer).”[1]
- STs were originally defined by Payne and Martin in 1990 as "traumatic injuries that can result in partial or full separation of the skin’s outer layers, that is, the separation of the epidermis from the dermis (partial thickness wound), or both the epidermis and dermis from the underlying structures (full thickness wound)".[5]
- STs are acute wounds with the potential to be closed by primary intention.[1] They can be further defined as uncomplicated or complicated [1][6]:
- Uncomplicated: An uncomplicated ST is an acute wound that heals within approximately 4 weeks.
- Complicated: A complicated ST is a complex, chronic wound that does not heal within 4 weeks.
Relevance
- STs occur with the highest frequency in the elderly population. Individuals in this age group might not live in satisfactory conditions, and some conditions may predispose the individual to increased risk for these wounds.
- STs may increase the length of hospitalization, increase health costs and have an impact on quality of life.[1]
- As individuals live longer, prevalence and incidence of STs are likely to increase, along with direct costs (e.g. treatment) and indirect costs (e.g. decreased quality of life). Thus, it is critical that healthcare professionals receive appropriate training in recognizing risk factors and creating effective care plans.
Epidemiology
Incidence
By care setting
- Long-term care: The incidence of STs among elderly people living in long-term care facilities has been reported to range between 2.23 to 92%.[2][3]
- In Japan, a study including 382 residents of a long-term care facility reported a ST incidence of 3.8%, mostly located on the forearm.[2]
- A systematic review of 5 studies reported an incidence rate ranging from 2.23% to 92% in long-stay institutions. The most significant risk factors were: advanced age, sequelae of reduced mobility, falls and injuries resulting from accidents, previous skin injuries, cognitive deficits/dementia, reliance on transfers.[3]
By anatomical area
- STs are more common on the extremities, particularly the upper extremities [4][7]
By age
- Although STs can occur in any age group, it is most prevalent in age extremes (elderly and very young) [8][9]
Prevalence
True prevalence of STs is not well understood.[10] Existing studies report prevalence varying from 3.9% and 26% [4][11][12][13][14][15]
By country
- U.S.: prevalence estimated to be between 9 and 33% in long-term care facilities [6][7]
- Canada: 14.7% [16][15]
- Denmark: 4.6% among residents of a long-term care facility. [14]
- Brazil: 3.3% among patients with cancer [17] and 11.6% among residents of a long-term care facility. [3]
By care setting
- Long-term care: 4.6 and 33%[6][7][14]
- Palliative care: 30% [6]
- Community: 20% [6]
- Pediatric acute care: 17% [6]
Risk Factors
Risk factors for development of STs
Development of STs depends on extrinsic and intrinsic factors [1][18]
- Intrinsic factors: physiologic or pathologic changes that result in more fragile, furrowed and/or wrinkled skin more prone to STs (e.g., extremes of age - newborns and very elderly, malnutrition)
- Extrinsic factors: external/environmental factors that increase risk for STs (e.g., reduced mobility requiring assisted transfers, increased exposure to mechanical trauma)
The International Skin Tear Advisory Panel (ISTAP) groups risk factors in three categories [4]:
- General health: chronic and critical disease, polypharmacy, cognitive, sensory, visual and auditory impairment and nutritional status
- Mobility: history of falls, impaired mobility, dependence for activities of daily living (ADLs) and mechanical trauma
- Skin: extremes of age, fragile skin and previous STs
According to a 2017 systematic review, the most prevalent risk factor for STs was old age, followed by impaired mobility, falls and accidental injuries, previous STs, cognitive deficit/dementia, dependence in transfers, and upper limbs.[3]
Table 1 below summarizes risk factors for development of STs, according to ISTAP and other studies.[4][16]
Table 1. Risk factors for development of skin tears.[4][16]
General Health
|
- Chronic and critical disease, for instance:
- Cardiac disorders
- Pulmonary disorders
- Incontinence/continence
- Limb edema
- Polypharmacy: Polypharmacy is the use of multiple medications which can predispose the sick person to drug interactions, drug reactions or confusion particularly in elderly patients. Polypharmacy has been associated to increased risk for confusion and falls in the elderly population, which links polypharmacy to a potentially heightened ST risk.
- Medications that may affect skin integrity, for instance:
- Use of corticosteroids
- Antineoplastic agents
- Cognitive: Altered levels of cognition in elderly persons, children and individuals with chronic and critical illnesses lead to an increased risk of developing ST. Aggressive behavior, agitation associated with altered cognition and the presence of dementia favor the risk of trauma and self-injury resulting in ST.
- Visual/ hearing deficiencies: Chronic and critical diseases and extremes of age can lead to sensory, auditory and visual changes. Aging may put the patient at risk of skin injury, slow wound healing and increase the risk of chronic diseases (diabetes, dementia and vascular disease). Sensory, auditory and visual changes have a strong link with episodes of falls, which lead to the occurrence of friction injuries.
- Nutritional status: Both obese and undernourished patients may be at risk for ST. [19]
|
Mobility
|
- History of falls: A fall is defined as a sudden and unintentional change in the position of the body. Factors that predispose to falls are diverse, such as: unstable gait and balance, muscular weakness, impaired vision, use of medications, dementia, carpets, disorganization of the environment, poorly adapted shoes, inadequate illumination, urinary urgency and neurological diseases. These factors contribute to the increased risk of STs with each fall.
- Conditions that decrease mobility, for instance:
- Muscle weakness
- Spasticity
- Hemiplegia/paraplegia
- Need for assistance with activities of daily living (ADLs): Activities of daily living include day to day routine such as: wearing clothes, bathing, positioning and transfers. Individuals often acquire STs during these daily activities, especially with those that depend on the assistance of another person.
- Mechanical trauma:
- Bumping into furniture or wheelchair pedals
- Skin trauma when putting on/taking off socks
|
Skin
|
- Skin changes related to extremes of age and critical illness
- Elderly (>75 years): with aging, the skin suffers changes such as atrophy of the subcutaneous tissue especially of the hands, legs and plantar region of the feet. Reduction of elasticity, resistance and moisture, senile purpura and inappropriate skin cleansing products are factors which make the skin vulnerable and susceptible to STs.
- Previous history of ST (see Figures 1 and 2)
- Sun damage
- Increased risk of pressure injuries
- Ecchymosis (see Figure 3)
- Senile purpura (see Figure 4)
- Vascular disorders
- Dry/ desquamating and fragile skin
- Mechanical trauma due to removal of adhesive tapes
- Skin cleansing products
- Inadequate use of skin protective barriers
|
Figures 1 to 4. Risk factors for development of skin tears

Fig. 1. Skin tear scar (star shaped scars) on elbow | 
Fig. 2. Skin tear scar (star shaped scars) on forearm |

Fig. 3. Ecchymosis on forearm | 
Fig. 4. Senile purpura |
Risk Assessment Tool
- 1CFor all patients, expert consensus recommends that clinicians perform a risk assessment for skin tears upon admission, daily (or periodically per facility policy) and after identification of an episode of ST to prevent new STs (Grade 1C).[1][6][16]
- Rationale: Recognition of at-risk patients is the first step in prevention. [1][6][16] While a validated risk assessment tool for ST does not exist yet, the ISTAP developed a risk assessment protocol based on expert consensus (evidence level C).[4] The pathway is composed of the three categories. The presence of one of more factors indicates that the individual is at-risk, prompting risk reduction interventions (Figure 5).[1][16] For preventative interventions, see section 'Prevention' in topic "Skin Tear - Treatment and Prevention".
- For long-term care facilities in the U.S., the Centers for Medicare and Medicaid Services (CMS) considers ST a potentially preventable event.[20] Once a potentially preventable event is identified in the facility (e.g. a patient with ST), CMS requires implementation of a corrective action, such as a performance improvement plan. If not implemented, the facility will be cited as non-compliant upon audits, and thus the importance of early detection through a risk assessment tool.[20]
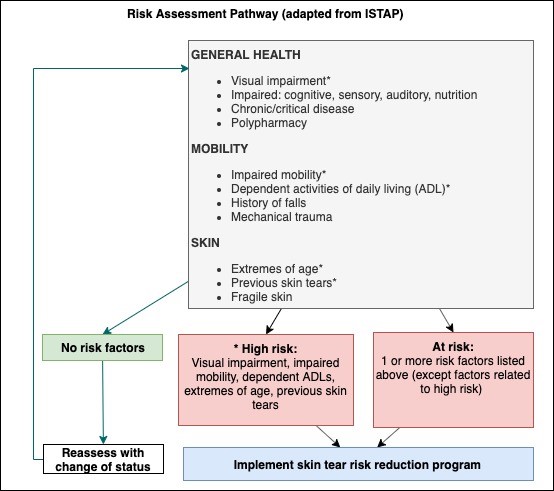
Fig. 5. Skin tear risk assessment pathway (adapted from LeBlanc et al, 2013)[4]
Etiology
STs are caused by a combination of intrinsic and extrinsic factors detailed above, which ultimately results in shear and friction. For identification, documentation and prevention purposes, it is important to establish the exact cause of the wound.
- Almost half of the STs are found without any apparent cause.[4]
- Among elderly, main documented causes are blunt trauma, activities of daily living (ADL), dressing/treatment related, falls, patient transfers, equipment injury.[4]
- Among children, medical adhesives is reported to be among the main cause.[16]
Pathophysiology
As the skin ages, epidermal and dermal layers become thinner and more susceptible to damage from mechanical forces such as friction and shearing (Figure 6).
Dermal thinning results in reduction of the blood supply to the area, along with reduction of the number of nerve endings and collagen. These changes lead to decreased sensation, temperature, tightness and moisture control, and increased propensity for lesions such as ecchymosis and senile purpura.
As previously stated, ST occurs when an extrinsic factor (e.g. mechanical trauma from adhesive tape, bed rails, furniture edges, wheelchairs) leads to frictional forces that are greater than those tolerated by the skin.[5]
- STs may occur due to shearing, attrition or blunt trauma, leading to:
- Detachment of the epidermis from the dermis (partial thickness wound) OR
- Detachment of the epidermis and dermis from the underlying structures (full thickness wound)
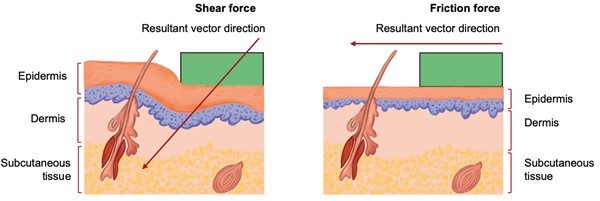
Fig. 6. Mechanical forces involved in the pathophysiology of a skin tear
ASSESSMENT
This section focuses on ST-specific elements that need to be included in a comprehensive assessment of patients with ST, based on recommendations from the ISTAP.[1]
Patients with STs need a comprehensive initial assessment to guide development of the most appropriate management plan and monitor wound healing progress. The initial assessment should include a complete history and physical examination, as well as evaluation of the wound.
Primary goals of assessment are:
- To identify underlying causes of the ST
- To identify risk factors for the development of ST or that may impede healing (if healing is a realistic goal)
- To identify pertinent patient's/caregivers' concerns
- To rule out other types of wounds, which may require different treatments. See 'Differential Diagnoses'
- To classify the ST
- To determine healability, that is, if the ST has potential to heal with conservative interventions only. See topic "How to Determine Healability of a Chronic Wound".
See Algorithm for Assessment of Skin Tears below (Algorithm 1)
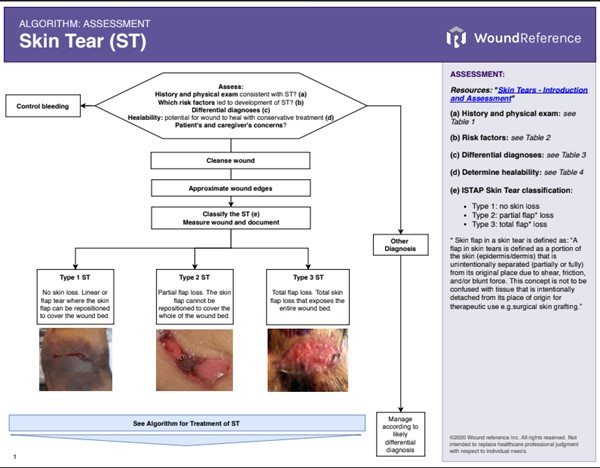
Algorithm 1. Assessment of Skin Tears
History
The non-exhaustive checklist below highlights relevant factors that should be assessed when taking history of a patient with a ST. Risk factors for the development of ST are indicated with the icon , risk factors for infection are indicated with
Chief Complaint and History of Present Illness
- Age, gender: extremes of age
- Onset of wound: usually acute
- Location of wound: most frequently occurs on limbs, especially upper extremity
- Cause of the wound:
- In elderly, one of the main causes is mechanical trauma during ADL (e.g. bumping into furniture or wheelchair pedals, putting on/taking off socks, use/removal of adhesive tapes, transfers and falls, use of restraints, use of orthotics) [6]
- In children, medical adhesives are among the main causes
- Pain
- History of previous ST
- History of falls
- Prior treatment/prevention
Medications
- Medications that impair wound healing include anticoagulants, antimicrobials (various antibiotic classes), anti-angiogenesis agents (eg, bevacizumab, aflibercept), antineoplastic drugs, anti-rheumatoid drugs (eg, methotrexate, aspirin/nonsteroidal anti-inflammatory drugs [NSAIDs]), colchicine (anti-gout drug), topical hydrogen peroxide, topical iodine, full-strength 0.5% Dakin’s solution (sodium hypochlorite), nicotine, steroids, and vasoconstrictors.[21][22][23]
- Polypharmacy: the use of multiple medications that might predispose patients to drug interactions/reactions or confusion
Social History
- Dependent ADL
- Smoking, drugs, alcohol may directly or indirectly impair wound healing [21]
- Social and caregivers' support, support at home
Review of Systems
- General:
- Nutrition status: malnutrition and hydration deficits
- Immunosuppression: auto-immune disease, immunosuppressants, malignancy
- HEENT: visual, auditory impairment
- Cardiovascular: hypertension/hypotension, hemodynamic instability, poor diffuse or localized blood perfusion (e.g. generalized atherosclerosis or lower extremity arterial insufficiency), or use of vasopressor infusion
- Neurological:
- Cognitive, sensory impairment
- Musculoskeletal:
- Psychiatric:
- Mental health issues
- Psychosocial and quality of life factors
- Skin:
- Presence of senile purpura, photo-aging, fragile skin and diseases, etc [6]
- Local edema, lymphedema, scars, erythema, ecchymosis, dermatitis, signs of abuse or neglect
Patient's and caregivers' concerns
Patient's and caregiver's concerns and psychosocial aspects should be assessed and taken into consideration when creating a treatment/prevention plan. Concerns and psychosocial aspects include but are not limited to [4]:
- Pain
- Ability/fear of carrying out ADL
Nutritional Assessment
- Expert consensus recommends a nutritional assessment upon a ST patient's entry to a new healthcare setting and whenever there is a change in the individual's condition.[1]
- Standardized tools such as the "Nestlé MNA" and "Self-MNA®" by Nestlé can be used to facilitate initial assessment and follow up.
- Medicare Quality Payment Program, Quality Measure:
- "Process Measure: Nutritional Screening and Intervention Plan in Patients with Chronic Wounds and Ulcers"
- "Patient Reported Nutritional Assessment and Intervention Plan in Patients with Wounds and Ulcers"
- "Preventative Care and Screening: Body Mass Index (BMI) Screening and Follow-Up"
Physical Examination
Besides a thorough physical examination, focused physical examination that includes the following is recommended:
Wound Exam
The following should be assessed [1][24][16]:
- Location: STs occur mainly on the upper and lower limbs of elderly persons. Limbs should be carefully evaluated particularly in persons with history of recurrent STs and senile purpura (Figure 7).
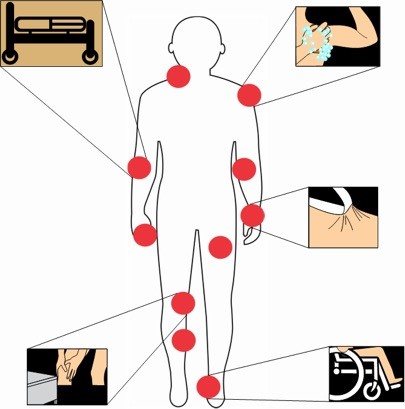
Fig. 7. Most frequent locations of skin tears
- Wound size: depth, width and length
- Wound bed characteristics and percentage of viable/non-viable tissue
- Wound edges: STs may present with a skin flap, which in this context refers to a portion of the skin (epidermis/dermis) that is unintentionally separated from its original place due to shear, friction and/or blunt force (and not intentionally detached from its place of origin for therapeutic use).[25] This flap may be realigned with the wound bed, and may appear pale, dark or viable
- Exudate type and quantity: seroanguineous exudate is always present at the beginning of the injury. STs may have an increased exudate in cases associated with comorbidities and uncontrolled edema
- Odor: presence of pus and malodor may be a sign of local wound infection
- Periwound skin: may have ecchymosis, edema and color changes
Diagnosis
Diagnosis of a ST is clinical, based on history and physical examination. Errors persist in the correct identification of STs, which results in underreporting, diagnostic errors and inadequate management of wound care. There is no consensus at the moment on the need for laboratory investigations or imaging to assist in the diagnosis of ST. [1]
Differential diagnosis
Differential diagnosis include stage 2 pressure ulcers/injuries, which generally occurs over bony prominences. Table 2 below contrasts characteristics of both conditions (Figures 8 and 9). Other differential diagnoses are deep tissue injury, incontinence-associated dermatitis, bruising, hematoma, terminal ulcers, and others. See topic "Pressure Ulcers/Injuries - Is it Really a Stage 2?"
Table 2. Comparison of Stage 2 pressure ulcer/injury and a skin tear
| Wound etiology/classification | Stage 2 Pressure Ulcer/Injury | Skin Tear |
| Image |  Fig. 8. Stage 2 pressure ulcer/injury Fig. 8. Stage 2 pressure ulcer/injury
|  Fig. 9. Skin tear (ISTAP type 2) Fig. 9. Skin tear (ISTAP type 2)
|
| Location | Generally on bony prominences.
| Upper and lower limbs, or in areas where adhesives have been used.
|
| Causes | Pressure, tissue tolerance, generally over bony prominences.
| Traumatic wound caused by mechanical forces, including the removal of adhesives.
|
| Characteristics | Can present as intact or open blister (bleb) filled with serous or serosanguinous fluid. | A skin flap may or may not be present.
|
| Exudate | Low exudate | Generally dry, but there may be situations that increase amount of exudate
|
Classification
Expert consensus recommends use of the ISTAP classification, as it is a widely used, validated method that uses a simple method to classify STs (Figures 10-12) [1][4][25]:
- Type 1 skin tear: No skin loss. Linear or flap tear where the skin flap can be repositioned to cover the wound bed.
- Type 2 skin tear: Partial flap loss. The skin flap cannot be repositioned to cover the whole of the wound bed.
- Type 3 skin tear: Total flap loss. Total skin flap loss that exposes the entire wound bed.
- Skin flap associated with the condition of a ST is defined as: “A flap in skin tears is defined as a portion of the skin (epidermis/dermis) that is unintentionally separated (partially or fully) from its original place due to shear, friction, and/or blunt force. This concept is not to be confused with tissue that is intentionally detached from its place of origin for therapeutic use e.g. surgical skin grafting.”[25]

Fig. 10. ISTAP type 1 skin tear
 Fig. 11. ISTAP type 2 skin tear
Fig. 11. ISTAP type 2 skin tear
 Fig. 12. ISTAP type 3 skin tear
Fig. 12. ISTAP type 3 skin tear
There are at least 2 other classification systems currently in use, but those are not as widespread as the ISTAP classification above:
- Payne-Martin classification system [5]: not validated, classifies ST according to the percentage of tissue loss. In practice, quantifying percentages of tissue loss may be difficult. [1]
- Category I: Skin tear without loss of tissue. The epidermal flap either completely covers the dermis or covers the dermis to within 1mm of the wound margin
- Ia: Linear type
- Ib: Flap type
- Category II: Skin tears with partial tissue loss
- IIa: Scant tissue loss (25% or less)
- IIb: Moderate to large loss of tissue (more than 25% loss of the epidermal flap)
- Category III: Skin tears with complete tissue loss
- STAR classification system [26]: modified version of the Payne-Martin scale. Although validated, it has not been widely utilized.[1]
Ulcer Healability (Prognosis)
Categorization of wound healability (i.e., healable, maintenance, or non-healable) is of particular importance.[16] This designation defines for the clinician, patient, and family an expected course of action, plan of care, and healing rate. As a prerequisite to setting realistic treatment objectives, wounds are differentiated as [16]:
- Healable wound: the cause is correctable, there is enough blood supply to heal; moist interactive healing
- Maintenance wound: the wound could heal, but the cause is not correctable due to various patient factors compromising wound healing at this time (e.g.: ST on a lower limb with uncontrolled edema)
- Non-healable wound: the ST has no ability to heal due to untreatable causes such as terminal illness or inadequate blood supply that is not bypassable or dilatable. In this case, goals for treatment include prevention of future STs or episodes of infection.
For a framework on identifying the potential for a wound to heal, see topic "How to Determine Healability of a Chronic Wound".
Complications
Although this type of wound is acute and superficial, it may develop into a chronic wound with delayed healing and increased risk of infection, cellulitis and sepsis. Some risk factors such as: nutritional status, use of anticoagulants, steroids, vascular and pulmonary disorders as well as incontinence represent potential risk factors for delayed wound healing or complications of these wounds. [27][28]
Documentation
Structured risk assessment should be documented upon first assessment and at subsequent evaluations. (See 'Risk Assessment Tool')
- Currently, there is no ICD-10 coding for STs. However, the ISTAP recommends that STs be recognized as a unique and complex wound etiology, distinct from other wound types.[1] For coding guidance, see section 'Coding' below.
- Documentation of assessment and care plan for patients with ST include:
- Assessment: ST risks, causes, location, size, depth (full thickness, partial thickness), wound characteristics (i.e., wound bed tissue type - eschar, fibrin, slough, granulation tissue, bleeding, exudate, odor, presence of skin flap), presence of pain/infection, as well as the appropriate ISTAP classification (see 'Classification' above) and patient's and caregiver's concerns. These factors guide recommendations for care, topical dressing and frequency of dressing changes [18]
- Care plan: interventions to treat the underlying cause and prevent further STs, local wound care interventions, skin care products used to treat or prevent STs (e.g. creams, lotions, acrylates, and non-traumatic dressings). It is also important to explore and document any barriers to adherence to care plan, including patient's or caregiver's refusal of a given intervention.
- Tools that facilitate standardized assessment and documentation should be used whenever possible:
- Wound assessment tools:
- Pressure Ulcer Scale for Healing (PUSH) Tool [29]
- Bates-Jensen Wound Assessment Tool [30]
- Wound imaging: digital photographs of PU/PI at the first consultation and periodically thereafter to document progress is helpful and ensures consistency of care among healthcare practitioners, facilitates telemedicine in remote areas, and illustrates improvement to the patient.
- Wound measurement: methods include manually measuring length and width (the longest length with the greatest width at right angles), manual tracing, digital photography, and software programs that calculate wound dimensions from a photograph of the lesion. Wound tracings that calculate the area via digital software are slightly better than linear measurement.[31]
CODING
ICD-10
- Currently, there is no ICD-10 code for STs.
- As ST is an acute wound, it is typically coded as a superficial injury. See codes in the 'Appendix - ICD-10 Coding'
- A ST may also be coded as a traumatic wound if it is large, if a skin flap has been lost (i.e. ISTAP type 3 skin tear), or if healing is delayed due to an underlying comorbidity.
Medicare MDS (long term care facilities)
- For Medicare patients treated at long-term care facilities in the U.S.:
- ST (M1040G) is a reportable skin condition under "Section M - Skin Conditions". [12][20] All STs are captured in item M1040G, regardless of the cause of the ST. Skin care products that are part of a resident's prevention or treatment care plan for STs (e.g. creams, lotions, acrylates, and non-traumatic dressings) need to be documented on MDS 3.0 section M, and needs to be captured on the appropriate part of M1200. [12]
Medicare OASIS (home health agencies)
- For Medicare patients under home health care in the U.S.:
- ST is a reportable condition under "Section J: Health Conditions" of the "Outcome and Assessment Information Set" (OASIS-D). If ST has been caused by a fall while patient is under home health care, it should be reported under Section J. [32]
APPENDIX
ICD-10 Coding
ICD-10 codes for superficial skin injury - skin tear / abrasion
Codes below should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail
- Ankle – S90.51XX
- Arm – S40.81XX
- Elbow – S50.31XX
- Face – S00.81XX
- Forearm – S50.81XX
- Fingers – S60.41XX
- Foot – S90.81XX
- Hand – S60.51XX
- Hip – S70.21XX
- Knee – S80.21XX
- Leg, Lower – S80.81XX
- Scalp – S00.01XX
- Shoulder – S40.21XX
- Toe(s) – S90.41XX
- Thigh – S70.31XX
- Thorax Wall, back – S20.41XX
- Thorax Wall, front – S20.31XX
- Wrist – S60.81XX