Last updated on 8/19/21 | First published on 4/28/18 | Literature review current through Jan. 2026
[cite]
Authors:
Elaine Horibe Song MD, PhD, MBA,
Tiffany Hamm BSN, RN, CWS, ACHRN, UHMSADS,
Jeff Mize RRT, CHT, UHMSADS,
Topic editors:
Cathy Milne APRN, MSN, CWOCN-AP,
Scott A. Robinson MD,
more...
Coauthor(s)
Elaine Horibe Song, MD, PhD, MBACo-Founder and Editor, Wound Reference, Inc;
Professor (Affiliate), Division of Plastic Surgery, Federal University of Sao Paulo;
Volunteer, Association for the Advancement of Wound Care;
Google Scholar Profile
Disclosures: Nothing to disclose
Jeff Mize, RRT, CHT, UHMSADS
Disclosures: Nothing to disclose
Tiffany Hamm, BSN, RN, CWS, ACHRN, UHMSADS
Chief Nursing Officer, Wound Reference, IncDisclosures: Nothing to disclose
Editors
Scott A. Robinson, MD
Disclosures: Nothing to disclose
Cathy Milne, APRN, MSN, CWOCN-AP
Disclosures: Nothing to disclose
For full access to this topic and more
premium content, upgrade today. Or get started with a Free Basic account (limited content and tools).
INTRODUCTION
Overview
Resting ankle-brachial index (ABI) is commonly used for detection of peripheral artery disease (PAD) in clinical settings. This topic provides indications, contraindications, step by step instructions, interpretation and information on CMS reimbursement for ABI exams.
For other noninvasive arterial tests, see section 'Noninvasive arterial tests' in topic "Arterial Ulcers - Introduction and Assessment".
Background
The ABI is a noninvasive arterial test for identifying lower extremity peripheral artery disease (PAD) (Figure 1). Narrowing of the lumen of the leg arteries decreases blood flow to the ankles, which in turn reduces the blood pressure in the ankle. The ABI is the result of dividing the highest pedal systolic pressure in the foot to the highest systolic pressure in the brachial arteries.[1] PAD is generally defined as an ABI < 0.90.[1]
Limitations of ABI include falsely elevated readings in patients with non-compressible arteries due to arterial calcification. Arterial calcification is often seen in patients with diabetes, renal insufficiency or advanced age.[2]
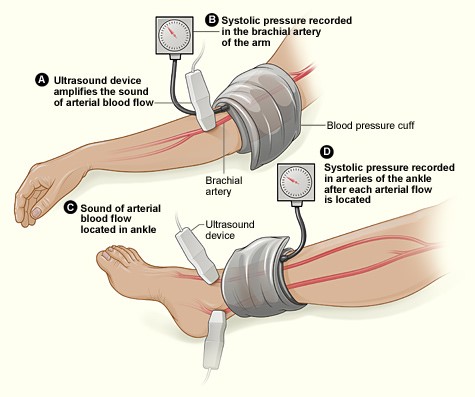
Fig. 1. Measuring the ankle brachial index with the Doppler method [3]
Indications
Symptomatic patients: to diagnose PAD
- For individuals with leg symptoms or signs that are suggestive of PAD, guidelines recommend ankle brachial index (ABI) and ankle pressure (AP) and as the first-line screening tests to diagnose PAD.[2][4][5]
- Signs and symptoms of PAD include [1] (See section 'Background' in topic "Arterial Ulcers - Introduction and Assessment"):
- Claudication symptoms: such as calf pain, leg weakness, other leg discomfort associated with activity and relieved by rest
- Chronic limb-threatening ischemia: chronic rest pain, ischemic ulcers or gangrene
- Acute limb ischemia: sudden painful, pale leg progressing to foot or leg paresthesia or paralysis
- ABI accuracy: the sensitivity and specificity of the ABI for detection of PAD with the Doppler technique range from 0.17 to 1.0 and from 0.80 to 1.0, respectively. Lower sensitivities (0.53–0.70) are reported in diabetic patients.[6][7]
- ABI limitations: for patients with diabetes mellitus, medial calcinosis, or end-stage renal disease, the American Heart Association (AHA) recommends other noninvasive tests to diagnose PAD, such as toe-brachial index or Doppler waveform.[6]
- Rationale: Diabetes mellitus, medial calcinosis, or end-stage renal disease lead to calcification of the arterial wall, which prevents detection of stenotic disease by the ABI. Vascular calcification causes the ankle artery to be incompressible and the systolic pressure at that location cannot be measured despite cuff inflation >250 mm Hg. In other cases, the ankle artery systolic pressure is measurable but is much higher than the brachial artery systolic pressure, leading to an ABI that exceeds the normal range.[6]
- For patients with an elevated ABI (>1.3), guidelines recommend measurement of the toe-brachial index.[5] The digital vessels rarely develop calcification and can provide an accurate determination of vascular disease in this setting.[5]
- For all patients with a non-healing wound or gangrene, the AHA suggests further assessment with other noninvasive arterial tests to rule out chronic limb-threatening ischemia (i.e, with toe brachial index with waveforms, transcutaneous oximetry, skin perfusion pressure), even if the initial ABI falls within normal range.[5]
- Rationale: Even if ABI results fall within normal range, it is important to note that values can be falsely elevated. This should be suspected if ABI is normal with a monophasic Doppler waveform or if non-healing wounds or gangrene are present.[2][8] See section 'Noninvasive arterial tests' in topic "Arterial Ulcers - Introduction and Assessment".
- For patients being considered for lower extremity compression therapy.
- The ABI rules out significant arterial disease and determines the amount of compression (if any) that can be applied safely. See topic "How to Select Adequate Compression Therapy Pressure Levels and Products".
Asymptomatic patients: to identify patients at risk for PAD
- For individuals at elevated cardiovascular risk without leg symptoms, clinicians might opt to use ABI to screen for PAD.[1][5]
- According to guidelines however, this patient population (patients with elevated cardiovascular risk without leg symptoms) warrants intensive atherosclerosis risk factor reduction regardless of the ABI, thus performing an ABI does not alter the care plan. In addition, the false positive rate is higher in this population, as the prevalence of PAD is lower in asymptomatic high cardiovascular risk patients than patients with leg symptoms.[1][5][9][10]
- For individuals at low or moderate cardiovascular risk without leg symptoms, guidelines do not support use of ABI to screen for PAD.[1][5][9][10]
Contraindications
- Deep vein thrombosis (DVT): the AHA guidelines recommend avoiding compression of the extremity with known or suspected DVT due to concern for breaking and embolizing a thrombus. [6]
- Inability to remain supine for the duration of the examination
- Extremity injury and other conditions (e.g. post mastectomy, post placement of a bypass graft) that prevent use of an occlusive sphygmomanometer
HOW TO PERFORM AN ABI
An ABI can provide three types of information:
- Numerical result: for interpretation of results, see section 'How to Interpret an ABI' below
- Doppler sound: sounds can be triphasic, biphasic and monophasic (see topic "How to Interpret Audible Handheld Doppler Ultrasound and Waveforms to Rule out PAD")
- Waveform: waveforms can be triphasic, biphasic and monophasic; waveforms show elasticity of the artery and its response to the blood flow (see topic "How to Interpret Audible Handheld Doppler Ultrasound and Waveforms to Rule out PAD")
Steps and Rationale
The steps below illustrate how to perform a single level ABI test [11] (billable with a CPT code 93922, if all requirements are met. See section 'Coding, Coverage and Reimbursement' below). See Figure 2.
| Process | Tasks | Rationale/ Tips |
Prepare equipment
| - Continuous wave vascular Doppler
- Probe (8 MHz probe for vessels near the surface like the radial, posterior tibial, and dorsalis pedis arteries)
- Straight segmental blood pressure cuffs (arms, legs, toe)
- Sphygmomanometer for inflating and deflating the vascular blood pressure cuffs
- Device that provides a hard-copy of the Doppler waveform (not analog)
- Conductivity gel
| - Select the appropriate sized cuff for each upper arm and for each ankle.
- The ideal cuff bladder length is ≥ 80 percent of the patient's arm circumference. The ideal cuff bladder width is ≥ 40 percent of the patient's arm circumference.[12]
|
| Prepare patient | - Patient should be supine, with the limbs at the same level as the heart (a rest period of 10 minutes is suggested). Remove patient's socks and any long sleeves. Ensure environment is warm.
| - Cold temperature and anxiety can lead to peripheral vasoconstriction, which interferes with the exam
- If patient is cold, provide a blanket
- Ensure patient is relaxed prior to taking ABI measurements (a rest period of 10 minutes is suggested)
|
Measure systolic pressure in the upper extremities
| - With the patient in supine position, place the blood pressure cuff on the right or left upper extremity
- Palpate the brachial pulse and apply conductivity gel where the pulse is felt
- Place the handheld Doppler on top of the gel at the brachial artery, at a 60 degree angle towards the patient's head
- Obtain a Doppler signal (sound) and waveform to establish a baseline
- Inflate the cuff to the point that the whooshing sound of the brachial pulse stops and continue inflating 20-30 mmHg above that point
- Slowly release the air from the cuff at 2-4 mmHg per second. When the heart sounds restart, note this as the brachial systolic pressure
- Repeat this process on the other arm. Use the higher of the two readings as the brachial pressure for the ABI calculation
|
|
Measure systolic pressure in the lower extremities
| - Place the cuff just above the malleoli on the lower leg.
- Locate the dorsalis pedis artery. Once you have palpated the pulse, apply gel on the spot and using the Doppler (angled towards the patient’s head about 60°) obtain the Doppler signal (sound) and waveform
- Inflate the cuff until the sound and waveform disappear and then inflate from 20-30 mmHg above that number
- Slowly release the air from the cuff at 2-4 mmHg per second. When the heart sounds restart, note this as the dorsalis pedis systolic pressure
- Deflate the cuff completely and record the systolic pressure for that site
- Locate the posterior tibial artery, 2-3 cm posterior to the medial malleolus. Repeat the procedure above and obtain the Doppler signal, waveform and systolic pressure.
- Measure and record systolic pressures of the dorsalis pedis and posterior tibial arteries of the contralateral leg
| - To locate the dorsalis pedis and posterior tibial arteries, see section 'Physical Examination - Palpation' in topic "Arterial Ulcers - Introduction and Assessment"
|
Calculate the ABI for each side
| To calculate the ABI: divide the higher ankle systolic pressure of each leg by the higher brachial pressure
- Right ABI = higher of the right-ankle blood pressure (right dorsalis pedis or right posterior tibial)/ higher brachial pressure
- Left ABI = higher of the left-ankle blood pressure (left dorsalis pedis or left posterior tibial)/ higher brachial pressure
| - Utilize the 'ABI worksheet' to record and calculate ABI
|

Fig. 2. Calculating the ankle-brachial index for each side
Video
- [External video] Ankle-brachial Index for Assessment of Peripheral Artery Disease
Worksheet
- Utilize the 'ABI worksheet' to record and calculate ABI
HOW TO INTERPRET AN ABI
ABI interpretation is shown below. For interpretation of other bedside non-invasive arterial tests, see section 'Noninvasive arterial tests' in topic "Arterial Ulcers - Introduction and Assessment".
| Interpretation | ABI (no diabetes) [13] | ABI (with diabetes)* [14] |
| Non-compressible arteries | >1.3 | >1.3 |
| No relevant ischemia | 0.8-1.3 | 0.9-1.3 |
| Mild/ Moderate ischemia | 0.4-0.79 | 0.5 -0.89 |
| Severe ischemia | <0.4 | <0.5 |
CODING, COVERAGE AND REIMBURSEMENT
Each individual Medicare insurance carrier determines the local coverage requirements for coverage of ABI. See local coverage determinations (LCD) related to noninvasive arterial tests in topic "Medicare Coverage Determinations for Wound Care".
Typically, Medicare considers an ABI part of the history and physical exam and thus does not cover ABI separately from an evaluation and management service.[15] However, an ABI may be reimbursed when derived from a more comprehensive procedure which includes a permanent chart copy of the measured pressures and waveforms in the examined vessels.[15] Note: Most Medicare carriers do not provide reimbursement for ankle waveforms generated by the older analog strip chart recorders, or for any device that does not provide a hard-copy of the waveform.
Some Medicare carriers (e.g. CGS) require an abnormal ABI before proceeding to more sophisticated or complete noninvasive arterial studies, except in patients with severe diabetes or uremia resulting in medial calcification as demonstrated by artifactually elevated ankle blood pressure.[15]
Medical necessity
In general Medicare considers noninvasive peripheral arterial examinations, performed to establish the level and/or degree of arterial occlusive disease, to be medically necessary if (1) significant signs and/or symptoms of possible limb ischemia are present and (2) the patient is a candidate for invasive/surgical therapeutic interventions.[15][16]
Some Medicare insurance carriers (e.g. Noridian) will require that noninvasive arterial and venous circulation in the extremity be confirmed within two weeks of the initial patient encounter and included in the treatment plan. Once adequacy of vascular supply is established, it is anticipated that these studies need not be repeated unless there is failure to achieve wound healing.[17]
CPT® Code
- CPT Code 93922: Limited bilateral noninvasive physiologic studies of upper or lower extremity arteries, (eg, for lower extremity: ankle/ brachial indices at distal posterior tibial and anterior tibial/ dorsalis pedis arteries plus bidirectional, doppler waveform recording and analysis at 1-2 levels, or ankle/brachial indices at distal posterior tibial and anterior tibial/dorsalis pedis arteries plus volume plethysmography at 1-2 levels, or ankle/ brachial indices at distal posterior tibial and anterior tibial/ dorsalis pedis arteries with transcutaneous oxygen tension measurements at 1-2 levels)
- When conducted at the ankle, this physiologic study has two components: 1) ABI values and 2) the bi- directional Doppler waveforms from the ankle (posterior tibial or dorsalis pedis arteries).
- CPT Code 93923: Complete bilateral noninvasive physiologic studies of upper or lower extremity arteries, 3 or more levels (eg, for lower extremity: ankle/brachial indices at distal posterior tibial and anterior tibial/dorsalis pedis arteries plus segmental blood pressure measurements with bidirectional doppler waveform recording and analysis, at 3 or more levels, or ankle/brachial indices at distal posterior tibial and anterior tibial/dorsalis pedis arteries plus segmental volume plethysmography at 3 or more levels, or ankle/brachial indices at distal posterior tibial and anterior tibial/dorsalis pedis arteries plus segmental transcutaneous oxygen tension measurements at 3 or more level(s), or single level study with provocative functional maneuvers (eg, measurements with postural provocative tests, or measurements with reactive hyperemia)
- CPT Code 93924: Noninvasive physiologic studies of lower extremity arteries, at rest and following treadmill stress testing, (ie, bidirectional doppler waveform or volume plethysmography recording and analysis at rest with ankle/brachial indices immediately after and at timed intervals following performance of a standardized protocol on a motorized treadmill plus recording of time of onset of claudication or other symptoms, maximal walking time, and time to recovery) complete bilateral study
Credentialing and Accreditation Standards
The accuracy of non-invasive vascular diagnostic studies depends on the knowledge, skill, and experience of the technologist and interpreter. Consequently, the physician performing and/or interpreting the study must be capable of demonstrating documented training and experience. A vascular diagnostic study may be personally performed by a physician, a certified technologist, or in a certified vascular testing lab.
Typically, CMS will consider services medically reasonable and necessary only if performed by appropriately trained providers (e.g. WPS's LCD).[18]
- Most Medicare carriers require non-invasive vascular diagnostic studies be performed meeting at least one of the following:
- performed by a licensed qualified physician, or
- performed by a technician who is certified in vascular technology, or
- performed in facilities with laboratories accredited in vascular technology
Official reprint from WoundReference® woundreference.com ©2026 Wound Reference, Inc. All Rights Reserved
Use of WoundReference is subject to the
Subscription and License Agreement.
NOTE: This is a controlled document. This document is not a substitute for proper training, experience, and exercising of professional judgment. While every effort has been made to ensure the accuracy of the contents, neither the authors nor the Wound Reference, Inc. give any guarantee as to the accuracy of the information contained in them nor accept any liability, with respect to loss, damage, injury or expense arising from any such errors or omissions in the contents of the work.
As a prerequisite to setting realistic treatment objectives, chronic wounds should be classified according to their ability to heal, that is, as healable, nonhealable, or maintenance. This designation defines for the clinician, patient, and family an expected course of action, plan of care, and healing rate. It also facilitates responsible use of available resources along with realistic treatment goals. This topic serves a tool to help clinicians assess wound healability.