Last updated on 3/14/24 | First published on 6/11/19 | Literature review current through Mar. 2025
[cite]
Authors:
Elaine Horibe Song MD, PhD, MBA,
Cathy Milne APRN, MSN, CWOCN-AP,
Amy Smith JD, RN, PHN,
more...
Coauthor(s)
Elaine Horibe Song, MD, PhD, MBACo-Founder and Editor, Wound Reference, Inc;
Professor (Affiliate), Division of Plastic Surgery, Federal University of Sao Paulo;
Volunteer, Association for the Advancement of Wound Care;
Google Scholar Profile
Disclosures: Nothing to disclose
Amy Smith, JD, RN, PHN
Disclosures: Nothing to disclose
Cathy Milne, APRN, MSN, CWOCN-AP
Disclosures: Nothing to disclose
Editors
ABSTRACT
Chronic wounds are a significant burden to individuals and healthcare systems, with "real world" healing rates of about 35%.[1] Wound healing is only one of the desirable outcomes in wound care. Often times wound healing is not a realistic goal (e.g., palliative cases), and other outcomes such as quality of life and pain control take priority. Whatever the target outcome might be, Quality is one of the cornerstones that can make the journey towards successful outcomes possible. This topic provides an update on Quality in wound care and how clinical decision support systems like WoundReference can help clinicians achieve better outcomes more efficiently. The topic lists resources such as a quality framework intended to be used for creation or assessment of wound care services, algorithms demonstrating application of evidence in product selection, quality measures specific to wound care, and guidance for wound and hyperbaric programs to successfully navigate the CMS Quality Payment Program (MIPS).
INTRODUCTION
Chronic wounds are a significant burden to individuals and healthcare systems. From 2014 to 2019, the number of Medicare beneficiaries in the United States with chronic ulcers rose from 14.5% to 16.4%.[2] The estimated yearly cost to Medicare for treating these chronic ulcers is around $22.5 billion.[2] While randomized controlled trials (RCTs) - which often exclude patients with serious other health issues - show a healing rate of 40%, real-world data from the U.S. Wound Registry (USWR) indicate an average healing rate of only about 35%.[1]
Wound healing is only one of the desirable outcomes in wound care. Often times wound healing is not a realistic goal (e.g., palliative cases), and other outcomes such as quality of life and pain control take priority. Whatever the target outcome might be, Quality is one of the cornerstones that can make the journey towards successful outcomes possible (Figure 1). This topic provides an update on Quality in wound care and how clinical decision support systems like WoundReference can help clinicians achieve better outcomes more efficiently.

Fig. 1. Quality and Outcomes
QUALITY IN WOUND CARE
What is Quality in healthcare and how can it improve outcomes?
Quality in healthcare
- Definition: According to the Health and Medicine Division (HMD), previously known as The Institute of Medicine, healthcare quality is defined as "the degree to which health care services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge." [3][4]
- The Health and Medicine Division further defines quality as having the following properties or domain [3][4]:
- Effectiveness. Relates to providing care processes and achieving outcomes as supported by scientific evidence.
- Efficiency. Relates to maximizing the quality of a comparable unit of health care delivered or unit of health benefit achieved for a given unit of health care resources used.
- Equity. Relates to providing health care of equal quality to those who may differ in personal characteristics other than their clinical condition or preferences for care.
- Patient-centeredness. Relates to meeting patients' needs and preferences and providing education and support.
- Safety. Relates to prevention of actual or potential bodily harm.
- Timeliness. Relates to obtaining needed care while minimizing delays.
Impact of Quality on outcomes in wound care
- Recognizing the need for a broadly applicable definition of quality in wound care, in 2006 the Association for Advancement of Wound Care (AAWC) created a framework for wound care quality that clearly illustrates the relationship between the aforementioned quality domains and outcomes in wound care. The framework, intended to be used to create or critique a wound care service delivery system, remains current and applicable to the socioeconomic reality in which patients and wound care clinicians live today.[5]
- The framework adapts the HMD's quality domains to wound management, presenting them as pillars over a foundation that represents the patient/ client with wounds. The concept of placing the patient at the base of the conceptual model facilitates patient empowerment and ownership in the decision-making processes related to wound management.[5] The six pillars represent aspects of Quality that together allow wound care clinicians to deliver patient-centric, optimized services through regulated/accredited healthcare organizations and achieve desired outcomes.
CLINICAL DECISION SUPPORT AND QUALITY IN WOUND CARE
How can clinical decision support systems enhance Quality and improve outcomes in wound care?
- Figure 2 summarizes the AAWC framework for wound care quality, and highlights how WoundReference clinical and reimbursement support platform supports and enables application of the framework in clinical practice.
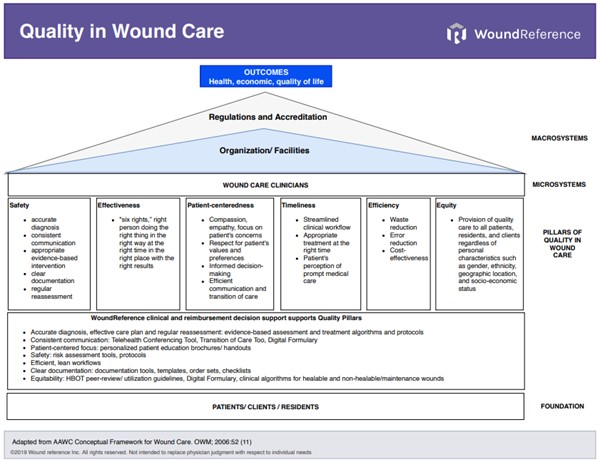
Pillars of Quality in Wound Care
The six pillars of Quality in Wound Care and related WoundReference decision support tools are listed below [5]:
1. Safety
According to the AAWC, the practice of safe wound care includes the items in bold below:
- Accurate diagnosis (or a working diagnosis)
- Consistent communication
- Clear documentation
- Documentation must meet the requirements of patients and of regulatory bodies that support and facilitate care. WoundReference streamlines documentation at the point-of-care with the Wound Prep and Dress Tool, medical necessity checklists, physician order sets, documentation templates in several topics of the Wound Care and Hyperbaric Oxygen Knowledge Base, risk assessment tools (e.g., Go-no-Go Tool)
- Regular re-assessment to ensure progress toward identified goals set between patient and provider
- Re-assessment ensures that the updated patient status clearly reinforces or alters the current plan of care. Triggers for reassessment of care plan are embedded in WoundReference's treatment algorithms, and hyperbaric oxygen therapy protocols. See Wound Care and Hyperbaric Oxygen Knowledge Base.
- Appropriate evidence-based intervention
- “Evidence-based clinical practice is an approach to decision making in which the clinician uses the best evidence available, in consultation with the patient, to decide upon the option which suits that patient best.”[5]
- Consistent use of evidence‐based practice protocols for each of the wound types is likely to enhance patient outcomes.[6]
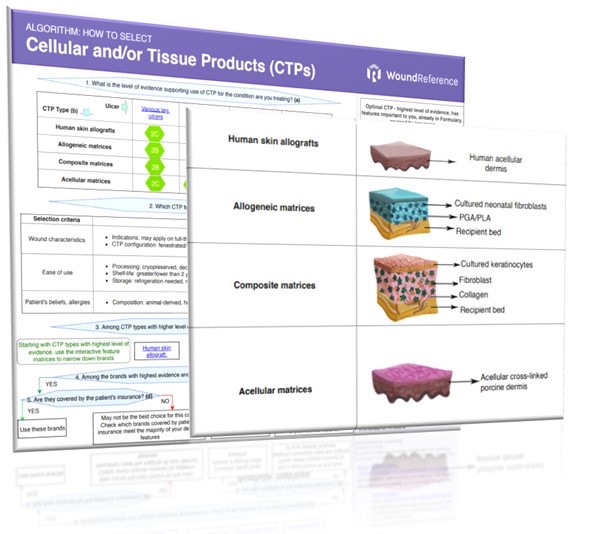
- WoundReference monitors clinical and reimbursement databases to ensure recommendations are always based on evidence and current. To ensure quality of recommendations, the editorial board follows a modified GRADE approach, a systematic methodology to rating the certainty of evidence in systematic reviews and other evidence syntheses.[7] Recommendations are embedded in the Wound Care and Hyperbaric Oxygen Knowledge Base and in tools such as the Wound Prep and Dress Tool. An example of how evidence is applied in practice is illustrated on the algorithm on Figure 3 (downloadable).
2. Wound care effectiveness
- The six components of clinical effectiveness are the “six rights,” including the right person doing the right thing in the right way at the right time in the right place with the right results.[8][5]
- Effectiveness can be greatly enhanced by point-of-care clinical decision support systems like WoundReference. As an example, USWR data suggest that point-of-care decision support and DFU quality measure reporting, even in the absence of a fiduciary incentive for practitioners can improve "real world" DFU healing rates by 10%.[1] See section 'Quality Measures in Wound Care' below.
3. Patient-centered wound care
- A shift from provider-centered towards patient-centered care has been observed recently. New care models have been encouraged by several regulatory bodies worldwide. Patients play a central role in their care, participating in discussions and helping plan/implement their treatment.
- Patients who are well-informed and actively participate in their wound care decision-making process tend to be more satisfied with the care they receive.[6]
4. Timeliness in wound care
- In wound care, "time is tissue". Timeliness comprises three components: patient's perception of prompt medical care, streamlined clinical workflow without unnecessary delays, and appropriate treatment at the right time. Failure to treat in a timely manner at any of the various stages in the disease process affects disease outcomes.[5]
- In the Netherlands, where around 17.5 million people live, it is estimated that prompt triage, analysis, and treatment of underlying causes of chronic wounds in a multidisciplinary setting could save approximately $145.8 million to $316.4 million in annual healthcare costs.[9]
5. Efficiency in wound care
- Efficiency is the relationship between patient care and the resources required to deliver it. The most obvious way to increase efficiency is to reduce waste.[5]
- WoundReference relies on the lean management approach to develop workflows, algorithms and tools. Lean, originally developed by Toyota Manufacturing, is a tool set, a management system that focuses on people and a philosophy that can change the way healthcare organizations are organized and managed.[10] The key goals of lean are to eliminate waste, value employees and continually improve the quality of services delivered to the customer/patient. It is value driven care with the patient as the central focus. An example of how waste can be reduced in wound care is the implementation of a Digital Formulary to create and manage local wound care formularies. See topic "Improving Wound Care with a Lean Approach".
6. Equity in wound care
- Equitable wound care is defined as providing quality care to all patients, residents, and clients regardless of personal characteristics such as gender, ethnicity, geographic location, and socio-economic status. [5]
- Wound care expenditures are a significant burden to healthcare systems, in part due to inappropriate over-utilization of high-cost resources and interventions. WoundReference's algorithms are developed so as to encourage appropriate, equitable distribution of resources among patients and satisfy individual needs in a cost-effective way. The digital Formulary Module also contributes toward equitable wound management, by saving financial and human resources, decreasing waste and reducing total treatment cost per episode of care.
Competency Assessments and Quality of care
- Regulatory agencies such as The Joint Commission (TJC) and the Undersea and Hyperbaric Medical Society (UHMS) lay out guidelines to implement processes to ensure that clinicians and providers are competent when performing patient care.
- Clinical decision support can help clinicians prepare for Competency Evaluations. Competency is best assessed via return demonstration and observation; additional methods include, but are not limited to, simulation, mock reviews and case studies.
QUALITY MEASURES IN WOUND CARE
"If you can’t measure it, you can’t improve it."
This quote is credited to Peter Drucker, a leader in modern business management. His quote is also applicable to healthcare, including wound care (Figure 4).

Fig. 4. Measuring quality
According to CMS, "quality measures are tools that help us measure or quantify healthcare processes, outcomes, patient perceptions, and organizational structure and/or systems that are associated with the ability to provide high-quality health care and/or that relate to one or more quality goals for healthcare."
However, wound care is not a recognized medical specialty.[1] As a result, a robust set of quality measures applicable across different care settings is yet to be developed. Wound care-relevant quality measures do exist, but have been developed by different organizations and are often not applicable to all care settings.
To ensure managers and clinicians can easily find and adopt wound care-relevant quality measures in clinical practice, WoundReference is the only online platform that provides the following resources for quality measures simultaneously:
- MY Power Search (select tab "Web", and click on filter "CMS Measures"): displays wound care-relevant measures, pulled from the Centers for Medicare and Medicaid Services (CMS) Measures Inventory
- Assessment and treatment algorithms and topics (Wound Care and Hyperbaric Oxygen Knowledge Base): allows clinicians to meet quality measures as they follow evidence-based workflows and protocols.
- Tables with quality measures related to specific conditions and interventions, as shown in the sample topics below:
- Tools for creation of balanced scorecards (BSCs): BSCs have been used in healthcare as a tool to plan and implement quality improvement initiatives, and participate in quality programs introduced by payers (e.g.Centers for Medicare & Medicaid Services - CMS Quality Programs).[11][12][13] See topic "Applying the Balanced Scorecard in Wound Management and Hyperbaric Medicine"
CMS QUALITY PAYMENT PROGRAM
In the United States, eligible wound care and hyperbaric providers who meet certain criteria and serve Medicare Part B patients who are furnished covered professional services under the Medicare Physician Fee Schedule are required to participate in the CMS Quality Payment Program (QPP) (Figure 5).

Fig. 5. The Centers for Medicare and Medicaid Services (CMS) Quality Payment Program
- Definition: the CMS QPP is a quality payment incentive program, which rewards value and outcomes in one of two ways: Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs).
- Purpose: the CMS QPP was designed to tie payments to quality and cost efficient care, drive improvement in care processes and health outcomes, increase the use of healthcare information, and reduce the cost of care.
- MIPS eligible clinician types:
- Physicians (including doctors of medicine, osteopathy, dental surgery, dental medicine, podiatric medicine, and optometry)
- Osteopathic practitioners
- Chiropractors
- Physician assistants
- Nurse practitioners
- Clinical nurse specialists
- Certified registered nurse anesthetists
- Physical therapists
- Occupational therapists
- Clinical psychologists
- Qualified speech-language pathologists
- Qualified audiologists
- Registered dietitians or nutrition professionals
- Clinical social workers
- Certified nurse midwives
If an eligible clinician does not participate in QPP, then he/she is subject to negative payment adjustments.
WoundReference clinical and reimbursement decision support can empower eligible clinicians and groups to maximize performance in MIPS. See more information on "MIPS in Wound Care and Hyperbaric Medicine" and "MIPS in Wound Care and Hyperbaric Medicine - Improvement Activities", or contact us.
Official reprint from WoundReference® woundreference.com ©2025 Wound Reference, Inc. All Rights Reserved
NOTE: This is a controlled document. This document is not a substitute for proper training, experience, and exercising of professional judgment. While every effort has been made to ensure the accuracy of the contents, neither the authors nor the Wound Reference, Inc. give any guarantee as to the accuracy of the information contained in them nor accept any liability, with respect to loss, damage, injury or expense arising from any such errors or omissions in the contents of the work.