Last updated on 9/1/22 | First published on 8/14/19 | Literature review current through Jan. 2026
[cite]
Authors:
Jeff Mize RRT, CHT, UHMSADS,
Tiffany Hamm BSN, RN, CWS, ACHRN, UHMSADS,
Eugene Worth MD, M.Ed., FABA, ABPM/UHM,
more...
Coauthor(s)
Jeff Mize, RRT, CHT, UHMSADS
Disclosures: Nothing to disclose
Tiffany Hamm, BSN, RN, CWS, ACHRN, UHMSADS
Chief Nursing Officer, Wound Reference, IncDisclosures: Nothing to disclose
Eugene Worth, MD, M.Ed., FABA, ABPM/UHM
Disclosures: Nothing to disclose
Editors
For full access to this topic and more
premium content, upgrade today. Or get started with a Free Basic account (limited content and tools).
INTRODUCTION
Providers must ensure that the termination of the patient relationship does not constitute abandonment. For example, the Kansas Court of Appeals has defined patient abandonment as: “[. . .] true abandonment - a medical practitioner’s discontinuance of services before the need for them is at an end and without due notice to the patient to afford him or her ample time to secure other professional attendance of his or her own choice”.
Providers should use caution when terminating a patient-provider relationship. Federal and state laws prohibit discrimination based on race, religion, color, etc., and other laws - such as the Americans with Disabilities Act (ADA) - may also apply. When confronted with a situation in which these laws might be applicable, providers should seek legal advice and consult with their institution's Risk Management or Corporate Compliance Department.
In circumstances where the provider is the sole practitioner of a certain specialty in an area or is practicing in a rural area, it may take longer to ensure a patient has appropriate care, which may result in a longer notice period prior to terminating the relationship.
Healthcare providers have the right to decide for whom they will provide care. Healthcare providers also have the right to terminate relationships with patients for a variety of reasons, such as:
- Numerous attempts at communication have proven unsuccessful.
- The patient has repeatedly refused to obtain needed screening or treatment.
- The patient is persistently rude or belligerent to providers and/or staff.
- Violent/ threatening behavior
- Lost or stolen prescriptions
- Unauthorized dependent drug dose escalation
- Appointment cancellations/no shows
- Early refill requests or asking to replace a visit with a refill
- Unexplainable urine drug testing results
- Soliciting prescriptions from other prescribers, including unauthorized ER visits
In all cases, careful specific documentation must be made in the medical record to describe relevant behaviors, their differential diagnosis and evaluation, and communication(s) with patients. Sometimes this communication/confrontation would be better made to a Hospital Ethics Committee if that option is available.
In some instances, even though the relationship with a patient or family might be problematic, the provider may not be ready to terminate the relationship. In these cases, the provider may consider using a behavior contract with the patient and/or family. A behavior contract can help preserve the provider-patient relationship, or - if the behavior contract is not followed - it can support the decision to terminate the relationship. Again, proper documentation in the patient's medical record supports the contemporaneous documentation of behavior over time.
We encourage the patient, provider and staff to be factual in documenting behavioral actions and acting out. This is no time to interject personal opinions or comments into the patient record. These may be seen as degrading and dehumanizing. As a famous television detective has said, "Just the facts, m
a'am."
LEGAL/ RISK MANAGEMENT CONSIDERATIONS
- To avoid charges of medical abandonment, discrimination, civil rights, or Americans with Disability Act violations, etc., patient dismissals must be non-discriminatory and should not jeopardize patient well-being.
- If appropriate, dismissals may include referral to a nearby Wound Care/ Hyperbaric provider if not already done.
- ANY DISMISSAL ACTIVITY MUST GO THROUGH RISK MANAGEMENT. If a provider or service is considering a patient dismissal, a call to the risk management office is recommended. The discussion and action plan as a result of this phone call, must be recorded in the patient record. The medical record note establishes the facts that the provider or service has made contact with Risk Management and that they have suggested a prudent course of action.
- Healthcare providers should review managed care contracts or other procedural documents prior to withdrawing from a patient’s care. It is quite possible that the patient can only come to this service (your clinic) because of insurance requirements. In that case, you must continue to provide care.
- Managed care organizations (MCOs) may require compliance with additional steps before a provider can unilaterally dismiss a patient from his or her care.
- MCOs may require warning letters or an extended waiting period to ensure that the patient has adequate time to select another provider from the MCO panel. Often, the MCO will seek to refer the patient to another provider within its network.
Your phone call with Risk Management should address this concern.
- Additionally, some state health programs may have special grievance procedures that healthcare providers must follow (e.g., Medicaid services).
- Each practice should research contractual and legal obligations before finalizing their discharge policies.
DOCUMENTATION
When the provider–patient relationship becomes untenable, the provider should review the patient's record before deciding to dismiss the patient. Although it is true that healthcare providers can terminate a relationship with a patient, it also is wise for the provider to have objective and factual documentation that supports the decision. For example:
- Have patient instructions and education been documented in the patient’s record?
- Have patient complaints or accusations against the practice, or inappropriate remarks to providers or staff, been documented? These issues should be objectively noted in the record; use quotation marks where relevant to preserve the patient's actual statements.
- Does documentation objectively note that the provider and staff have attempted to resolve the problems or address the issues?
- Has the provider consistently documented treatment recommendations and warnings to the patient about possible negative effects of noncompliance? (Note: Noncompliance should be documented at the time it occurs, not when the patient sustains an injury.)
If the record provides no support for the decision to terminate the relationship, then the provider may choose to continue treating the patient, at least until such time as the documentation supports the decision.
OPERATIONAL GUIDELINES
The following is operational guidance for termination of a patient-provider relationship. Proper discharge of a patient from a provider’s practice should include the following elements:
- If dismissal is agreed upon, the patient will be sent/given a termination letter.
- The Provider and the Practice Manager must sign the letter with a copy to the Practice Director.
- The dismissal is done in writing, via delivery that confirms receipt to the patient, such as certified mail or hand-delivery.
- In the dismissal letter the provider agrees to provide 15-30 days of emergency coverage while the patient obtains a new provider.
- If possible, the provider provides referral information to the patient regarding possible new providers.
- Notification in the letter to the patient that patient records will be sent to the new provider upon receipt of written authorization from the patient.
- Notification of dismissal should be sent as certified mail, return receipt requested, restricted delivery in compliance with HIPAA. If the patient refuses the certified letter:
- Document the patient’s refusal to accept the certified letter.
- Scan and keep a copy of the unaccepted letter, including the return receipt.
- Forward the actual unaccepted letter including the return receipt to health information management (HIM) for inclusion in the patient’s hard copy record.
Terminating a patient-physician relationship is never fun. But in our experience, the termination process is much easier if a standardized approach is followed for all challenging relationships.
SAMPLE PATIENT DISMISSAL LETTER
Below is a sample patient dismissal letter. It can be altered as needed to meet underlying circumstances, such as whether the 30 day requirement is waved due to threatening behavior, whether refills will be provided during this time.
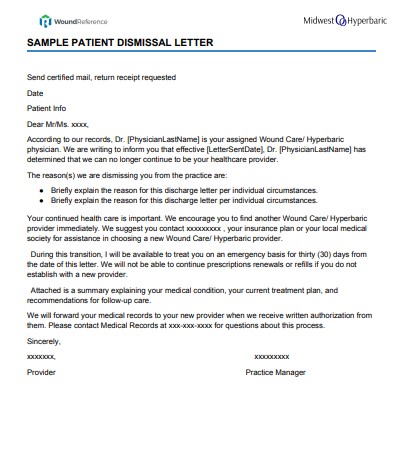
Sample patient dismissal letter
Official reprint from WoundReference® woundreference.com ©2026 Wound Reference, Inc. All Rights Reserved
NOTE: This is a controlled document. This document is not a substitute for proper training, experience, and exercising of professional judgment. While every effort has been made to ensure the accuracy of the contents, neither the authors nor the Wound Reference, Inc. give any guarantee as to the accuracy of the information contained in them nor accept any liability, with respect to loss, damage, injury or expense arising from any such errors or omissions in the contents of the work.