|
Conservative Sharp Wound Debridement Documentation Checklist and Template | Videos
|
CLINICAL
Overview
According to guidelines adopted by the Centers for Medicare and Medicaid Services (CMS), the different methods of wound debridement include selective (e.g., sharp debridement), non-selective (mechanical, enzymatic, autolytic or larval), or surgical.[1][2][3][4][5][6] This document focuses specifically on conservative sharp wound debridement (CSWD), which is considered a selective method of debridement. For a review on different types of wound debridement, see topic “Debridement”.
Background
- CSWD is a quick and efficient debridement method that may be associated with significant risk to the patient if performed inappropriately.[7]
- CSWD should be part of a comprehensive care plan that addresses patient concerns, treats causes that led to the wound, and provides adequate local wound care.
Definition
-
-
Wound debridement: is the process of removing necrotic or nonviable tissue and biofilm from pressure ulcers, burns, and other acute and chronic wounds to for the purpose of exposing healthy tissue.[8][9] Debridement may be categorized as selective, non-selective or surgical (excisional).[1][2][3][4][5][6] The context in which CSWD fits into the spectrum of debridement options is described below. For definitions of non-selective and surgical debridement, see topic “Debridement”.
-
-
- Selective Debridement (CPTs 97597 and 97598) is the removal of specific, targeted areas of devitalized or necrotic tissue from a wound along the margin of viable tissue by high-pressure waterjet with/without suction, sharp dissection/debridement utilizing scissors, scalpel, curettes, and/or tweezers/forceps. This procedure typically requires no or limited topical or local anesthesia and generally has minimal associated bleeding.
-
-
Selective conservative sharp wound debridement (CSWD): is the removal of specific, targeted areas of devitalized or necrotic tissue from a wound along/above the margin of viable tissue, utilizing sharp instruments such as scissors, scalpel, curettes, and/or tweezers/forceps.[1][2][3][4][5][6][8][9] Minimal pain and bleeding are expected with CSWD and repeated debridement is often needed.[8][9][10]
-
Differences between CSWD and surgical debridement: CSWD is not as aggressive as surgical (also known as excisional) wound debridement performed by physicians and other qualified healthcare professionals (QHPs), who remove devitalized tissue down to a viable, bleeding wound bed; this typically requires local, regional or general anesthesia.[9][11][12][13] Of note, the routine application of a topical or local anesthetic does not elevate the procedure from active wound care management or selective CSWD to surgical debridement.[2] For details on differences among types of debridement see section 'Types of debridement' in "Debridement".
Care Settings
CSWD may be performed in a multitude of care settings, including inpatient hospital, outpatient hospital, home health, skilled nursing facilities, etc. For details on coding, coverage, and reimbursement, see section below 'Coding and Reimbursement'.
Regardless of the care setting, when performing CSWD, clinicians should ensure that the:
- Facility has policies in place to allow nurses and other clinicians to perform CSWD.[14]
- Clinician performing the procedure has been appropriately trained, and competency has been updated as per facility requirements.
- Clinician has facility privileges and is allowed to perform CSWD as per facility policies.
- Care setting has sufficient resources to address potential complications.
- Patient provides written or verbal informed consent as required by facility policies.
Scope of Practice in the U.S.
- Scope of practice concerning CSWD differs from that of surgical sharp debridement in that [13]:
-
- Surgical sharp debridement privileges are limited to physicians and other QHPs, depending on state board regulations.
- CSWD may be performed by physicians and other clinicians, as determined by state boards’ regulations and facility policies.[3]
-
- A physician’s or advanced practice registered nurses’ (depending on each state) order is required to perform CSWD.
- Regulations on what type of healthcare professionals can perform CSWD vary from state to state. Regulations may change, thus healthcare professionals should consult the individual state practice act prior to performing CSWD.[13]
-
- For instance, with regard to nursing, each state’s Nurse Practice Act or Board of Nursing dictates specific regulations for this procedure.[13]
- For a summary of regulations and links to board of nursing organizations by state see topic "State-by-State Regulations on Conservative Sharp Debridement by Nurses in the United States"
Skills and Education
- Requirements for performing CSWD include specific education, training and demonstration of competency in CSWD according to licensure, and facility policy and procedures.[9][14][10]
- Some State Boards of Nursing require completion of a course on debridement (courses can be found by searching online for “courses on conservative sharp debridement’). Continued competency requirements shall include but are not limited to [9][14][14][10][15]:
-
- infection control procedures;
- types of debridement;
- wound etiology and disease process;
- complications;
- terminology;
- pharmacology pertaining to medications utilized in debridement;
- skin and tissue anatomy and physiology; see section 'Understanding Relevant Tissue Anatomy' below
- skill competency validation.
Understanding Relevant Tissue Anatomy
Knowledge of the skin and relevant tissue anatomy is a requirement prior to performing CSWD. Timely recognition of underlying anatomical structures such as bone, tendon, fascia, muscle, ligaments, vessels and nerves can help prevent unintentional damage during CSWD. Those structures should not be disturbed during CSWD. If any of these structures is cut or injured during CSWD, immediate physician involvement is warranted.[7] Figures 1 to 6 below illustrate examples of anatomical structures that may be encountered during CSWD.
|
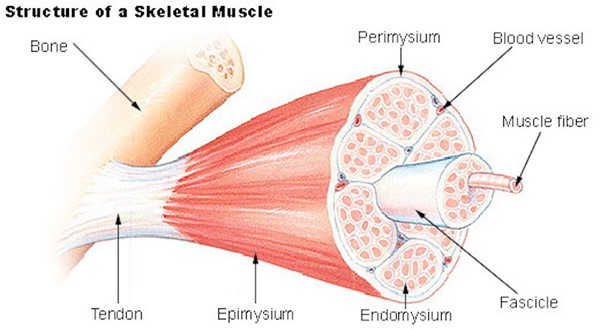
Fig. 1. Schematic showing muscle, tendon, bone
|
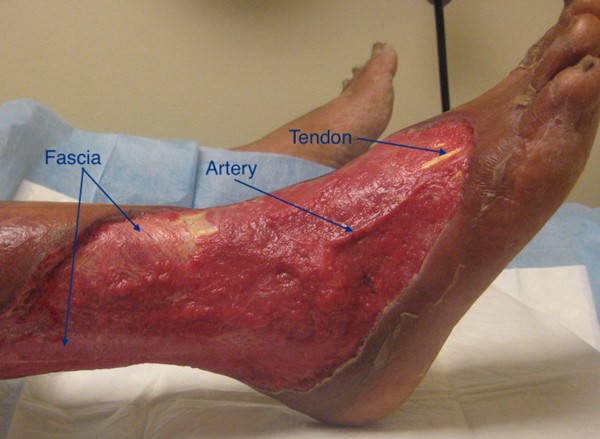
Fig. 2. Traumatic wound with exposed fascia, artery, tendons. By Lebendiskaya, N.
|
|

Fig. 3. Wound bed with fibrin covering underlying fascia. By Lebendiskaya, N.
|

Fig. 4. Wound bed with exposed muscle. By Lebendiskaya, N.
|
|

Fig. 5. Ulcer with exposed bone, perforated to promote growth of granulation tissue. By Lebendiskaya, N.
|
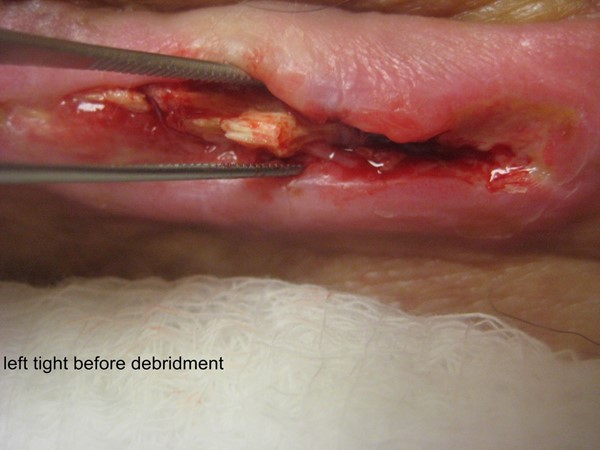
Fig. 6. Calcium deposit on wound bed. By Lebendiskaya, N.
|
General Indications and Contraindications
When assessing for indications and contraindications for CSWD, it is important to first determine the potential for functional healing of the wound. See topic "How to Determine Healability of a Chronic Wound".
- For wounds whose underlying causes cannot be immediately corrected or if there is inadequate blood supply to heal (i.e., maintenance or non-healable wounds), CSWD of slough may be performed if no contraindications exist.
- For healable wounds, surgical debridement is an appropriate method of initial debridement, if available as an option.[16] CSWD may be performed subsequently, or if surgical debridement is not an option or contraindicated.[7]
Indications
In general, indications for CSWD include [9]:
- Presence of necrotic tissue as well as cellular or proteinaceous debris [2][17]
- Various types of acute and chronic wounds: pressure, neuropathic/diabetic, and venous leg ulcers requiring removal of any nonviable tissue
- Callus on the foot or at the margins of a non-ischemic diabetic foot ulcer [7]
- Presence of bioburden, biofilm and/or local wound infection [7]
CSWD should be performed with caution and in collaboration with a physician or advanced practice registered nurse in a controlled setting in the following situations [7]:
- Patient is at risk for increased bleeding (e.g., use of anticoagulants)
- Moderate or severe peripheral arterial disease is present
- Patient has significant wound pain or pain associated with CSWD
- Wound has exposed bones, ligaments or tendons
- Devitalized tissue is over a major blood vessel, organ or structure
Contraindications
Contraindications to CSWD include [9][12]:
- Inability to determine interface between viable and nonviable tissue
- Extensive undermining or tunneling
- Abscess (if present, incision and drainage is initially indicated; may be followed by CSWD as needed)
- Dry, stable heel ulcers
- Stable, ischemic wounds
- Dry, stable (densely adherent) eschar
- Advancing cellulitis or sepsis, in which case surgical debridement is preferred
- Malignant cutaneous wounds such as fungating tumors
- Pyoderma gangrenosum or vasculitic ulcers, in which case debridement may exacerbate the condition. See topic "Pyoderma Gangrenosum - Introduction and Assessment"
- Wounds on face, hands, and feet near nerves, vascular structures, grafts, prostheses, dialysis fistulae, or joints
- Patient does not consent to CSWD
Ideal Frequency
The appropriate interval and frequency of debridement depends on the individual clinical characteristics of the patient and the extent of the wound. The extent and number of services provided should be medically necessary and reasonable based on the documented medical evaluation of the patient's condition, diagnosis, and plan.[2]
In the U.S., some Local Coverage Determinations state that for DFUs, debridement more frequently than once every seven (7) days, for a period longer than three months may not be reasonable and necessary, and therefore may not be eligible for reimbursement.[4]
-
For chronic wounds with biofilm, consensus guidelines suggest clinicians perform repeated maintenance debridement at every dressing change [18]
-
-
Rationale: Experts strongly agree that surgical or CSWD are both effective methods in removing biofilm.[18] However, it is difficult to remove all biofilm, and mature biofilms can regrow as soon as within 24 hours post-debridement. Thus, in order to suppress biofilm reformation the consensus suggests that debridement be performed repeatedly and be followed by application of topical antiseptic within the initial 24 hours post-debridement.[18] Initially, CSWD may be performed weekly, then at longer intervals as wound shows signs of improvement.
-
For large wounds, if quantity of non-viable tissue is extensive or more difficult to remove, clinicians may consider consecutive serial debridements in order to partially remove the necrotic tissue at each time.[7][12]
-
-
Rationale: Keeping length of the procedure between 15 to 30 minutes helps prevent nurse and patient fatigue.[7][12]
HOW TO PERFORM CONSERVATIVE SHARP WOUND DEBRIDEMENT
Assessment
CSWD is part of a comprehensive care plan. Prior to performing CSWD, it is important that a comprehensive assessment be performed so that the following questions can be answered:
- Is the wound healable?
- Is debridement indicated?
- Are there any contraindications?
- What are the risks and benefits for the patient?
The comprehensive assessment includes [7]:
- Patient’s and caregiver’s concerns
-
- Impact of CSWD on daily routine, quality of life, environment of care
- Pain assessment
- Wound healability (see topic "How to Determine Healability of a Chronic Wound")
-
- Comorbidities: conditions that increase the risk for bleeding (e.g. bleeding disorders), or delay wound healing (e.g. immunosuppression)
- Medications: use of medications that increase risk for bleeding (e.g, aspirin, anticoagulants) or delay healing (e.g. corticosteroids, etc)
- Lower limb assessment if the wound is on the leg or foot
-
- If signs or symptoms of peripheral artery disease, venous insufficiency, decreased sensation (i.e. neuropathy) are present, conduct a more in-depth lower limb assessment, beginning with non-invasive bedside arterial testing (e.g. ankle-brachial index - ABI)
- Detailed wound assessment
-
- History of current and previous wounds
- Etiology (e.g. CSWD on malignant or pathergic wounds is contraindicated)
- Location:
-
- Local anatomy: proximity to arteries, veins, nerves, tendons
- Proximity to vascular grafts, prostheses or dialysis fistulae
- Wound dimensions: length, width, area, depth
- Tunneling and undermining
- Wound bed: percentage of tissue type (eschar, fibrin/slough, granulation, epithelization), presence of a foreign body and/or exposed underlying structures, e.g. tendon, muscle or bone.
- Periwound: callus, maceration
- Visibility of interface between viable and nonviable tissue
- Type of material requiring debridement: fibrin/slough, eschar, callus, debris, biofilm
- Assessment for wound infection
-
- Bioburden, localized infection
- Spreading or systemic infection (if present, sharp surgical debridement is indicated)
Procedure
After determining that debridement is indicated via a thorough patient and focused wound assessment as described above, clinicians may utilize the following steps as a guide for performing CSWD.
Tables 1 to 3 below illustrate steps and rationale to appropriately perform CSWD before, during and after the procedure. [12][10][19][20]
Table 1. Pre-Procedure
| Steps |
Rationale/ Tips
|
|
1. Prior to performing any CSWD procedure, review individual clinician qualifications for CSWD including:
- Licensure and scope of practice
- Educational preparation
- Competency
- State organization regulations
- Individual facility policy and specific protocols related to CSWD
- Level of supervision required
-
- Confirm clinician performing procedure has privileges for CWSD. If supervision is required for the individual performing the procedure, ensure specific guidelines are followed.
|
- This addresses regulatory compliance as well as patient safety standards to ensure qualified individuals are participating in the procedure.
- Supervision of licensed professionals varies widely and facilities may define supervision as it relates best to their processes as they deem appropriate (e.g. supervision may be direct, or indirect).
- Facilities may specifically exclude clinicians from performing procedures unless a verified competency is maintained.
|
|
2. Confirm presence of an active order for CWSD by a qualified healthcare provider (e.g. advanced practice registered nurse, depending on state regulations)
|
- This ensures compliance in settings where individuals who are not qualified by licensure to order the procedure have active orders to perform the procedure.
|
3. Ensure correct patient identity per protocol.
|
- Facility policy will dictate how patient should be appropriately identified.
|
|
4. Confirm presence of informed consent, verbal or written per facility policy.
|
- Depending on setting and clinician performing CWSD, each procedural occurrence may require a separate consent.
- By obtaining informed consent, the patient is aware of the purpose for the procedure, benefits, as well as the expected outcomes and potential complications.
|
|
5. Ensure adequate assistance, supplies, and equipment:
- Appropriate lighting
- Assistive equipment/ additional personnel for positioning
- Personal protective equipment (PPE): clean gloves, eyewear, mask if desired
- Sharps container, bio-hazard disposable bag
- Sterile gauze, dressing supplies, absorbent underpads
- Hemostatic agent such as silver nitrate, cellulose sponges or alginate materials
- Sterile instruments such as forceps with and without teeth, #15 or #10 scalpel, curettes of different sizes, Metzenbaum and/or iris scissors (preferably curved), tissue nipper, rongeur for non-viable bone (Figure 7)

Fig. 7. Instruments for wound debridement
|
- Visualization is paramount to successful debridement, and poor lighting can obscure tissue planes; have a headlight available for difficult to illuminate areas.
- If additional personnel are required for ergonomic positioning during debridement, efforts should be made to secure assistance; discomfort on the part of clinician or patient during the procedure may lead to early cessation or suboptimal debridement.
- Know the hemostatic agents available in your facility, and how to obtain them.
- Ensure a variety of instruments are available for the procedure, as varying wound and tissue types will dictate the most useful instrument for the procedure; i.e. curette for flat, sporadically attached viscous/fibrotic material and exudates, or scissors for large collections of tissue which are easily elevated from the wound base.
- Absorbent underpads can be tucked into patient clothing to protect, as well as placed under the area of the wound to absorb cleansing fluid and drainage.
|
|
6. Ensure patient is positioned for comfort and adequately medicated for pain prior procedure. (For pain management, see section ‘Troubleshooting’ below)
|
- Although, by definition, CWSD should not involve excision of viable tissue, the patient may experience discomfort with disturbance of deeply seated/adherent tissue during retraction/removal necessary to perform procedure; patients that experience excessive pain when any pressure is exerted in the vicinity of the wound may not be good candidates for CSWD.
- Clinicians may elect to utilize oral pain medications, topical, or both.
|
Table 2. During the Procedure
| Steps |
Rationale/ Tips |
|
1. Perform hand hygiene, and don clean gloves.
|
- Literature evidence has not demonstrated that utilizing sterile technique for CSWD decreases incidence of wound infections.
- However, utilizing sterile instruments, supplies, and dressings is a universal, expected standard.
|
| 2. Open supplies onto separate surface or tray, in an area independent of patient or clinician movement. |
- Tools should never be placed on an unstable surface, such as the patient; this could potentially cause injury.
|
3. Conduct a procedure Time Out, per facility policy.
|
- This is a regulatory requirement at some facilities; it ensures the correct procedure is being performed on the correct patient, and that the consent matches the procedure being performed.
|
|
4. Cleanse wound and periwound with body temperature cleansing agent of choice, ensuring irrigation is performed at safe pressure.
- Irrigate with a device known to administer safe pressure for viable tissue (8-15PSI).[19]
|
- Ensure cleansing agent utilized is proven non-cytotoxic to healthy tissue; the overall goals of wound healing are to support healthy tissue while minimizing nonviable tissue.
- Some cleansers, though they possess strong antimicrobial action, can damage viable cells in the wound.
- Using safe PSI range ensures adequate cleansing without driving bacteria and debris further into the tissue or injuring viable tissue.
- Irrigation prior to debridement can also serve to loosen and hydrate nonviable tissue, facilitating debridement.
- The choice of antiseptic should consider wound type and location, exudate amount, likely organisms, contraindications (e.g., exposed cartilage), patient allergies, pain tolerance, and product cost or availability. The agent’s mechanism of action, contact time, and application frequency must follow manufacturer guidelines.[21]
- For instance, pure hypochlorous acid (pHA) is an oxidizing antiseptic effective against bacteria (including MRSA, VRE), fungi, viruses, and spores.[21] For optimal efficacy, a contact time of 10–15 minutes is recommended.[21] The wound and periwound may be cleansed with gauze soaked in approximately 2 mL of pHA for about 5 minutes before sharp debridement, and it may be used to irrigate the wound after debridement as well.[22]
|
|
5. Identify the target nonviable tissue for removal.
- If the tissue is pedunculated or mobile:
-
- Utilizing tissue forceps in the nondominant hand, grasp the visible nonviable tissue and retract away from the wound bed to apply traction and provide tension. It is ideal to begin the dissection at an area where the nonviable tissue is most mobile, or most easily distinguishable from viable tissue. The tissue forceps should be held like a pencil, with the thumb and the middle finger moving in a pincer motion to close the forceps (Figure 8)
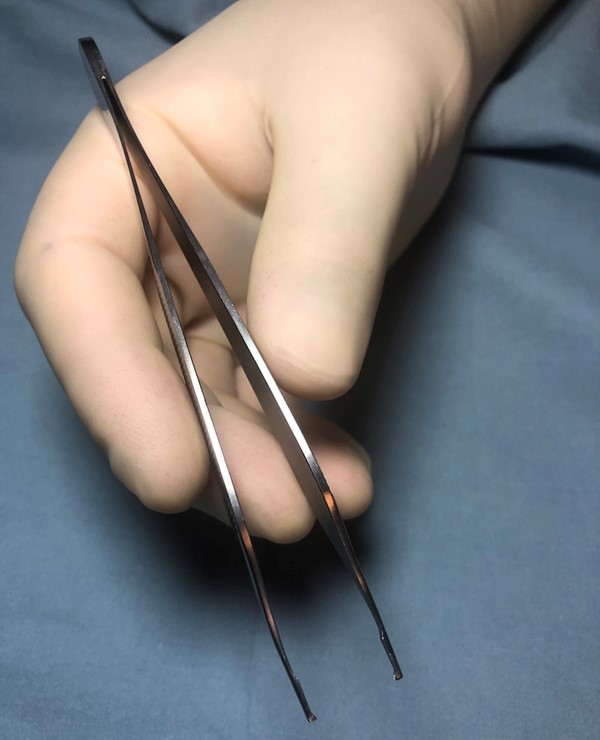
Fig. 8. Holding forceps
|
- This retraction and tension will allow easier identification and subsequent dissection of the tissue planes
|
|
6. If utilizing the #10 or #15 scalpel, or scissors, gently begin to separate and dissect the nonviable tissue at lowest visible point nearest the wound bed, always keeping the tip of the scalpel or scissors in view. The directional separation of the nonviable tissue should be tangential or angled upward away from the wound bed.
- A #15 blade will be held like a pencil, allowing the curved tip of the blade to contact the tissue; this can be used with a ‘picking’ motion, carefully cutting smaller areas of nonviable tissue.
- A #10 blade will be held in a similar manner, but slightly further back from the blade, allowing the largest area of the blade to contact the tissue; this can be used in a broader, sweeping motion over larger areas of nonviable tissue, utilizing the entire length of the cutting surface of the blade. (Figure 9)

Fig. 9. Holding a #10 blade scalpel
- Tissue scissors are held in a position with the thumb and ring fingers in the two rings of the instrument, with the middle finger resting where the shaft meets the ring, and the index finger on the screw of the articulating portion of the scissor, ideally the palm faces down, and if the scissors are curved, the tips should curve away from the wound bed and any viable tissue. (Figure 10) The tip of the scissors is the correct portion to utilize for cutting; if the jaws near the articulation area are used, the tip is not visible and could potentially cause injury. Scissors are best utilized for boggy tissue, where use of a curette or scalpel may require excessive pressure or force.
-
- The scissors can also be used to dissect bluntly by introducing the tip into the tissue and then spreading the jaws open; this often aids visualization of any potential structures past the visible surface of nonviable tissue.
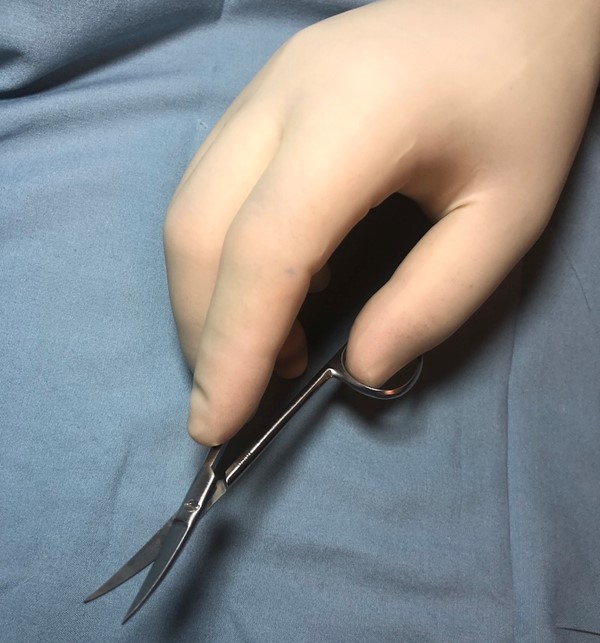
Fig. 10. Holding curved iris scissors
- If the target material identified for removal is more flush along the wound surface, a ring curette may be utilized. It can be held like a pencil, with the tip of the instrument pointed toward the wound with the sharp edge facing toward the clinician; this will be best utilized with a ‘painting’ motion, removing nonviable tissue by slowly separating layers of material. A bone curette, such as a Volkmann curette, may also be used in this manner for CSWD. (Video 1 below)
|
- Resting the working/dissecting hand on a surface, such as the patient or on the table, will steady the instrument in the event of sudden patient movement, and can provide greater accuracy.
- If the palm faces upward while using scissors for dissection, there may be inadvertent angling of the scissor tips in a downward fashion, risking removal of viable tissue.
|
7. Avoid any tissue that is not readily identifiable or any obvious vascular, or viable tissue structures, sutures, or graft material (unless intention is to specifically remove the suture or graft material).
- If bleeding occurs, see bleeding management in section ‘Troubleshooting’ below.
|
- Suture or other non-native materials can cause foreign body reaction or act as nidus for infection; these are only removed if they are separated from the living tissue and no longer performing the intended function for which they were placed. The operative note may be helpful in decision making. If in doubt, contact surgeon
|
8. Stop the procedure when no longer able to discern dissection plane between viable and nonviable tissue, or to further separate nonviable tissue from the wound bed, significant pain occurs, or when viable tissue and/or bleeding is encountered, the procedure should be concluded.
|
- If any of the listed conditions are met, any further attempts at debridement may result in nonselective debridement, which is no longer within the scope of the CSWD procedure.
|
|
9. Cleanse wound with cleansing agent of choice, ensuring irrigation is performed at safe pressure.
- Do NOT irrigate if hemostatic agents were required for hemostasis
|
- This ensures any additional detritus is removed from the wound environment, further decreasing the inflammatory response.
- Irrigation may dislodge fibrin clots.
- See Step 4. above for more tips on wound cleansing
|
10. Apply dressing per orders, or as desired.
|
|
Videos
Video 1. Conservative sharp wound debridement using curette. By S. Robinson, M.D. Wound does not have exposed tendons, bones, vessels or nerves. Topical anesthetic applied prior to the procedure.
Video 2. Conservative sharp wound debridement using curette. Focus on the sound of optimal debridement. By S. Robinson, M.D.
Table 3. Post-Procedure
| Steps |
Rationale/ Tips |
1. Complete required documentation as listed in section ‘Documentation’ below.
|
- Documentation should be thorough and consistent, describing each facet of the procedure; this is also imperative to optimize reimbursement.
|
2. Repeat steps as needed to remove nonviable tissue.
|
- See “How to Assess Effectiveness” below
|
Documentation
For a complete list of documentation requirements for debridement, see section 'Documentation Requirements' in topic "Debridement".
Following the conservative sharp wound debridement procedure, document the following [23][17] (see Conservative Sharp Wound Debridement Documentation Checklist and Template):
- Patient consent
- Medical diagnosis
- Location of the debridement:
-
- Anatomical site of wound
- Specificity is necessary when documenting debridement of multiple wounds
- Indication(s) and medical necessity for the debridement
- Debridement will be considered not reasonable and necessary for a wound that is clean and free of necrotic tissue/slough.[17]
- Debridement of extensive eczematous or infected skin is not appropriate for debridement of a localized amount of tissue normally associated with a circumscribed lesion. Examples of this are ulcers, furuncles, and localized skin infections.[17]
- Surgical debridement will be considered not reasonable and necessary when documentation indicates the wound is without devitalized, fibrotic, nonviable tissue, infection, necrosis, foreign matter, or if the wound has pink to red granulated tissue. When utilized, it is expected that the frequency of debridement will decrease over time.[17]
- The following services are considered to be not reasonable and necessary wound debridement services [17]:
- Removal of necrotic tissue by cleansing or dry-to-dry or wet-to-dry dressing.
- Washing bacterial or fungal debris from lesions.
- Removal of secretions and coagulation serum from normal skin surrounding an ulcer.
- Dressing of small or superficial lesions.
- Paring or cutting of corns or non-plantar calluses.
- Incision and drainage of abscess including paronychia, trimming or debridement of mycotic nails, avulsion of nail plates, acne surgery, or destruction of warts.
- Removal of non-tissue integrated fibrin exudates, crusts, or other materials from a wound without removal of tissue does not meet the definition of any debridement code and may not be reported as such.
- Type of anesthesia (if used), including route, length of application, and person administering (e.g., none, topical 1% lidocaine, 5% lidocaine, or other)
- Appearance of the wound prior to debridement such as:
-
- Pre-debridement dimensions: diameter, depth, area in centimeters
- Undermining or tunneling, wound bed tissue composition by percentage, color, presence of exudates or necrotic tissue, signs of infection, purulent drainage or abscess, visible structures such as bone, tendon, vessels or nerves
- Vascular status, or evidence of reduced circulation
- Narrative of the CSWD procedure to include:
-
- Method used for debridement (CSWD)
- Instruments used (e.g., scalpel, scissors, curette, etc)
- Wound debridement utilizing a method which is unproven by valid scientific literature would be considered investigational and not reasonable and necessary.[17]
- Statement that non-viable tissue was removed, and debridement was performed along/above the margins of viable tissue
- Level/depth of tissue debrided:
-
- Partial thickness,
- Full thickness,
- Subcutaneous tissue debridement,
- Subcutaneous tissue and muscle debridement,
- Subcutaneous tissue, muscle and bone debridement.
- Description of the types(s) of tissue involved and the tissue(s) removed.
-
- Epidermis
- Dermis
- Subcutaneous tissue
- Muscle
- Bone
- Presence of untoward events and treatment used:
-
- Pain during or following the procedure
- Bleeding if present especially if difficult to control. Hemostasis achieved?
- Any damage to underlying tissue
- Appearance of the wound following debridement including:
-
- Post-debridement dimensions,
- Description of any remaining non-viable material present, degree of epithelialization
- Other types of debridement performed on the wound.
- Type of dressing applied to the wound
- Photograph before and after debridement
- Date for follow-up assessment
- Date for follow-up debridement session, based on agency policy
- Other post procedure notes or patient teaching, including follow up instructions
Plan of Care
The medical record must include a plan of care containing treatment goals and physician or other qualified provider follow-up. The record must document complicating factors for wound healing as well as measures taken to control complicating factors when debridement is part of the plan.[17] A wound that shows no improvement after 30 days may require a new approach, which may include a physician reassessment of underlying infection, off-loading, biofilm, metabolic, nutritional, or vascular problems which may inhibit wound healing. It is expected the wound care treatment plan is modified in the event that appropriate healing is not achieved after serial debridement over 30 days.[17]
HOW TO ASSESS EFFECTIVENESS
Signs of effectiveness include:
- Increasing proportion of granulation tissue on wound bed and no signs or symptoms of infection
- Decrease in wound area, depth, exudate, necrotic tissue
Signs that CSWD is not being effective include:
- No increase in granulation tissue or improvement in wound dimensions upon serial examination/assessment
If the wound shows no signs of improvement within 30 days, clinicians should reassess the treatment approach. Documentation may include a physician/QHP reassessment of underlying infection, metabolic, nutritional, or vascular problems inhibiting wound healing, and a new treatment approach.[17]
TROUBLESHOOTING
Pain
- For patients with significant wound pain prior to the procedure, CSWD may not be indicated. Other methods may be preferred.
- For patients with wound pain prior to the procedure, for large wounds or if pain is anticipated, the following options are indicated:
-
- Oral analgesics: coordinate care so that medication is administered prior to CSWD, with sufficient time to obtain analgesia.
- Topical anesthetics:
- EMLA: EMLA has been shown to reduce pain and decrease the length of time needed to achieve a clear wound bed. [12] Apply 30-60 minutes ahead of CSWD on area to be debrided. Apply 1-2 grams per 10 cm2 (2 inches), up to 10 grams in total. Cover the wound with an occlusive dressing for 30-60 minutes, and debride immediately after removal of EMLA cream. [24]
- Lidocaine 4% gel: may be applied topically on the area to be debrided and covered with occlusive dressing (e.g. transparent film) for 5 minutes (onset 3-5 minutes)
- Local infiltrative anesthesia. For details, see topic "How to Administer Local Anesthesia for Wound Care Procedures".
-
Bleeding
- If bleeding occurs, isolate the source, using irrigation to clear the field and gauze to blot the area.
- If bleeding is generalized oozing:
-
- Apply pressure for 5 minutes. If bleeding slows but does not stop, apply cellulose foam or powder or alginate, cover with moist gauze, and apply pressure again for 5 minutes. Do NOT remove cellulose material after application; apply moist pressure dressing, monitor patient, and reassess to ensure hemostasis.
-
- Cellulose agents are physical barriers to bleeding, and therefore removal of these agents by wiping with gauze will negate their role in hemostasis; pressure over cellulose dressings should be carried out with a moist dressing as to not dislodge the material inadvertently.
- Silver nitrate may also be applied to the location of bleeding, rolling the tip of the applicator over the area for 15-30 seconds; this may be repeated 2-3 times.
-
- If silver nitrate is used, consider cleansing wound with sterile water as to not inactivate the agent (if desired).
- If bleeding is pulsatile:
-
- Alert supervising provider immediately, or take appropriate action per facility policy, licensure, and individual competency (e.g. topical application of epinephrine, electrocautery, suture ligation).
- Any bleeding not completely controlled within 15 minutes requires additional evaluation.
CODING AND REIMBURSEMENT
Medicare Administrative Contractors and Local Coverage Determinations
- See section "Medicare Administrative Contractors and Local Coverage Determinations" in topic "Debridement"
CPT Codes
- 97597 Deb (e.g, high pressure waterjet with / without suction, sharp selective debridement with scissors, scalpel and forceps), open wound (e.g. fibrin, devitalized epidermis and/or dermis, exudate, debridement, biofilm), including topical application(s), wound assessment, use of a whirlpool, when performed and instruction(s) for ongoing care, per session, total wound(s) surface area, first 20 SQ CM or Less.
- 97598 Deb (e.g, high pressure waterjet with / without suction, sharp selective debridement with scissors, scalpel and forceps), open wound (e.g. fibrin, devitalized epidermis and/or dermis, exudate, debridement, biofilm), including topical application(s), wound assessment, use of a whirlpool, when performed and instruction(s) for ongoing care, per session, total wound(s) surface area, each additional 20 SQ CM, or part thereof (list separately in addition to code for primary procedure)
Billing Tips
- CSWD versus surgical sharp debridement (CPT 11042-11047) [2][3]:
- Do not bill CPT 97597 and 97598 with CPT 11042-11047.
- When deciding which code to use, the deepest layer of viable tissue removed (e.g., skin, subcutaneous tissue, muscle, etc) determines the appropriate code. For example, when only biofilm on the surface of a muscular ulceration is debrided, then codes 97597-97598 would be appropriate. If viable muscle substance was debrided, the 11043-11046 series would be appropriate, depending on the surface area.[2][3]
- For detailed guidance, see section 'Types of Debridement' in topic "Debridement".
- Debridement and Unna boot
- All supply items related to the Unna boot are inclusive in the reimbursement for CPT code 29580. When both a debridement is performed and an Unna boot is applied, only the debridement may be reimbursed. If only an Unna boot is applied and the wound is not debrided, then only the Unna boot application may be eligible for reimbursement. The National Correct Coding Initiative (NCCI) Policy Manual for Medicare Services Chapter 4, section G states that debridement codes (11042-11047, 97597) should not be reported with codes 29580, 29581 for the same anatomic area. [2]
- Place of service:
-
-
Skilled nursing facility (SNF): do not bill Medicare for debridement services performed on Medicare beneficiaries receiving Medicare Part A-covered care in a SNF. CPT 97597 and 97598 codes in a skilled nursing facility setting are part of the Medicare Part A skilled nursing facility consolidated billing protocols. Therefore, you should discuss this with nursing facilities for direct payment from them for these services.[25]
-
Home health (HH): CSWD services performed by physical therapists on Medicare beneficiaries under a HH benefit who have CSWD listed in their Plan of Care are included in the consolidated home health billing and are not reimbursed separately. When CSWD services are delivered by physicians or QHPs, services may be separately reimbursed by Medicare Part B, even if the beneficiary is under an active HH plan of care. See CMS Publication 100-02, Medicare Coverage Policy Manual, Chapter 7 – Home Health Services, Section 10.10 – Consolidated Billing, C. Relationship Between Consolidated Billing Requirements and Part B Supplies and Part B Therapies Included in the Baseline Rates That Could Have Been Unbundled Prior to HH PPS That No Longer Can Be Unbundled which states. [26][27]