ABSTRACT
Creating and maintaining an environment of safety in the hyperbaric facility is achieved through proactive planning and attention to detail. Lack of proper safety protocols and procedures causes accidents, and, unfortunately, loss of life. While we never want to have a disaster, we learn from safety analysis of them.
This topic provides a summarized update on Safety in the Hyperbaric Facility. The topic also provides guidance and resources that will help you build an excellent hyperbaric safety program. Resources include safety guidelines, job descriptions, go-no-go lists, go-no-go risk assessment tool, and emergency procedures.
INTRODUCTION
Individual experience and the recounted experiences of documented mishaps within hyperbaric facilities demonstrate the need to be proactive in our preparation. For example, actively practicing emergency procedures is paramount to ensuring the safety of the staff and patients. Through active practice and debriefing, we create an environment of safety in our clinics and hyperbaric oxygen facilities. These procedures should involve all personnel within the clinic and sometimes beyond. In fact, we know of facilities who arrange with hospital security and the local firehouse to create a 'realistic' fire drill that involves rolling the fire trucks, pulling hose, and evacuating 'patients.'
Explore some of the safety tools and content for free and stay informed. For full access, see Plans. SAFETY PROGRAM GUIDELINES
As required in NFPA 99, Chapter 14, each clinical hyperbaric facility must designate a Safety Director. The Role of the Hyperbaric Safety Director is to ensure that processes and systems are in place to proactively reduce risk and mitigate loss. The knowledge and experience required for the job should comply with the guidelines set forth in the staffing and training recommendations listed below. In accordance with the requirements set forth in NFPA 99, Chapter 14, the Safety Director will work with the governing body of the parent organization and the Hyperbaric Medical Director in order to develop a comprehensive safety program for all permanent and part-time department personnel.[1]
The foundation of every hyperbaric facility is their Hyperbaric Safety Program.
The following guidelines must be established in place to promote high standards of patient care and operational safety within the hyperbaric program. At minimum, the Safety Program must include the following elements [1]:
- Documented safety procedures, which must address general facility safety, specific chamber related operational safety procedures (e.g., fire in the chamber, patient evacuation, contaminated air, and equipment failure). It must also address physiological reactions and complications (e.g., ear pain, sinus pain, oxygen toxicity reactions, or claustrophobia).
- Documented recurring in-service training for all hyperbaric facility staff on selected safety topics. Training sessions shall consist of (but not limited to) fire drills, mock patient emergencies, simulated equipment failure, simulated contaminated breathing gas, updates on codes and standards.
- Documented preventive maintenance program executed either by local technical personnel or by a third-party maintenance contractor.
- Documented major maintenance program for specific hyperbaric facility components such as (but not limited to) compressors, control components, fire suppression system components, etc. (as appropriate).
- All full- and part-time hyperbaric facility personnel must be aware of the potential hazards associated with the operation of clinical hyperbaric chambers and their related support systems. All technical personnel must pursue continuing education credits in various aspects of hyperbaric facility safety. Refer to UHMS approved hyperbaric facility safety director training.[2]
Hyperbaric facility safety is the responsibility of everyone directly or indirectly involved in the clinical hyperbaric medicine program.
For more information on safety guidelines, see topic "Safety Program Guidelines".
MEDICAL DIRECTOR GUIDELINES
The Medical Director is responsible for the quality of hyperbaric services provided and is accountable to the medical staff and hospital administration for the activities of the hyperbaric center. In addition, the Medical Director is directly responsible to ensure the hyperbaric medicine service has appropriate medical coverage from a licensed provider who has received hyperbaric training and is appropriately credentialed by the hospital and hyperbaric medicine department. The medical director is a key individual in a hyperbaric medicine service. Not only important for staffing and day-to-day function, the medical director has an important role in the clinic and patient safety. For more information, see topics "Medical Director Guidelines" and "Medical Director Job Description".
DESIGNATION OF HYPERBARIC SAFETY DIRECTOR
A Hyperbaric Safety Director must be formally designated for each clinic/ hyperbaric facility. This designation includes requirements related to ongoing training and education of the hyperbaric team. We have referenced papers and hyperbaric safety authors who explain the rationale behind having a formally designated and specifically trained Safety Director in each hyperbaric medicine facility, even if a management organization has one Safety Director named at the corporate level for all of their facilities. The unit Safety Officer may not have a "director" title, due to HR constraints, but must be accorded a level of distinction above the standard hyperbaric technologists and chamber operators. Hyperbaric providers are encouraged to read this technical document in order to find out what applies to their facility, and why each facility should have its own designated safety director. This is key in order to comply with the intent and requirements of local, state, and national codes/ requirements. Designation of the Safety Director in writing with an appropriate job description for the role are paramount to hyperbaric facility safety. See topics "Designation of Hyperbaric Safety Director", and "Hyperbaric Safety Director".
HYPERBARIC PROGRAM STAFFING GUIDELINES
Determining the make-up of the hyperbaric team is dependent on the purpose and scope of the facility. A facility that is open 24/7x365 requires a wholly different level of staffing than a clinic open from 8:00 to 5:00, treating no after-hours emergencies. Nevertheless, regardless of the purpose and scope of the facility, minimum qualifications and training for hyperbaric personnel are the same and should be observed, in order to ensure patient/ staff safety and safeguard the program against medical-legal actions. Inadequate knowledge of applicable gas laws, chamber fire safety, potential risks, side effects, and contraindications of hyperbaric medicine, may result in dangerous situations that risk patient(s) and personnel well-being.
Regulatory and accreditation bodies such as the National Fire Protection Association (NFPA), the Undersea and Hyperbaric Medical Society (UHMS) and the National Board of Diving and Hyperbaric Medical Technology (NBDHMT) have an expectation that each hyperbaric medicine facility has appropriately trained personnel who are qualified to provide care and treatment in a safe manner. See topics "Staff Qualification" and "Staff Minimum Qualifications and Training for HBOT".
Staffing of the hyperbaric medicine department is the responsibility of the Nurse Manager and/or Program Manager, Medical Director with collaboration from the Safety Director to ensure compliance with the Safety Program Guidelines. The hyperbaric medicine team is a multidisciplinary group of healthcare professionals, institutionally credentialed with training and qualification(s) in the safe provision of hyperbaric oxygen therapy. It is necessary to identify the roles and responsibilities of the physician(s), nurses, and allied health professionals that staff the program. See topics "Staff Qualification" and "Staff Minimum Qualifications and Training for HBOT".
HBOT SAFETY INSPECTIONS
Providing hyperbaric oxygen therapy (HBOT) in a safe manner is our primary objective with each and every treatment. Clinicians providing HBOT go to great lengths to ensure patient safety with every treatment. In an article published on the NEJM Catalyst website, “Smartlists for Patients: The Next Frontier for Engagement?” Latif et al. identify that checklists work by providing information about who needs to act; what actions need to be taken; and how, where, and when each action should occur.[3] Indeed, customized patient-centered checklists have a wide range of applications, with the potential to improve patient education, pre-procedure planning, discharge instructions, care coordination, chronic care management, and plans for staying well. We utilize processes and systems that have been developed within the field, in some cases through “near misses” and accident analyses. We also apply standards set forth by The Joint Commission (TJC) and the Undersea and Hyperbaric Medical Society (UHMS).
With respect to chamber inspections, those should be conducted routinely in order to clarify proper chamber maintenance procedures and ensure safe operations of all equipment utilized during HBOT, and the safety of the environment in the hyperbaric medicine facility.
All equipment utilized by the hyperbaric medicine facility should be maintained through a program of regular preventative maintenance. The manufacturer is then responsible for the regularly scheduled service required to maintain the hyperbaric the physical chamber(s) and directly related ancillary equipment. Biomedical and other life sensitive equipment should be serviced and maintained by the hospital's biomedical engineering department. While this seems complicated, the division of responsibility is natural and based on the scope of practice for the facility. All of this equipment must be cleaned and maintained in accordance with the recommendations of the manufacturer. See topic "HBO Safety Inspections".
PROHIBITED ITEMS, RISK ASSESSMENT AND AUTHORIZATION
Wound dressings, devices and other objects that go in the hyperbaric chamber with the patient may raise important safety concerns, including production of heat, production of static electricity, production of flammable vapor, ignition temperature, and total fuel load. It is critical that clinicians understand which dressings, devices and objects are prohibited, restricted or allowed inside a hyperbaric chamber during HBOT.
Frequently, questions arise in regards to what can be taken into the chamber. The NFPA 99 2012 edition, chapter 14 Hyperbaric Facilities – provides the process for effectively managing patient care product(s) during hyperbaric oxygen therapy. The NFPA 99 2018 edition - 14.3.1.6.4.4 states “Physician and Safety Director approval to use prohibited items shall be stated in writing for all prohibited materials employed”. [4]
To facilitate assessment, the Go-No-Go assessment tool was created, as an interactive process that enables the user to document the product information necessary to complete the risk assessment process. The Go-No-Go Risk Assessment Tool is an interactive tool that facilitates the decision-making and documentation process. The Tool enables HBOT clinicians to assess the risk for each area of concern (production of heat, static, flash point, fuel load, adverse effect, mechanical), quantify each risk with the Burman scoring system, and more confidently determine the risk level of each item. Upon completion of the risk assessment process, HBOT clinicians can print or email the document and upload documentation to the electronic medical record. The Tool allows each facility to have a digital, customized "Go-No Go" list, that can be accessed by the entire team. For an overview of the Tool, watch the webinar "Performing risk assessments with the Go/No-Go Tool and the Burman Scoring System", and refer to topic "How to Assess HBOT Prohibited Items: The Go/No-Go Risk Assessment Tool And The Burman Scoring System". For challenges and solutions related to prohibited items risk assessment, see topic "Prohibited Item Risk Assessment".
For convenience, we also maintain a comprehensive, growing list of items that are approved for use, should be used with caution and should not be used in the chamber. See topic "Go-No-Go Lists / Prohibited Items" and "Go-No-Go : Frequently Asked Questions". An authorization form is required for items that should be used with caution (download sample form).
Also, refer to the poster "Fire Safety Time Out", which can be used to remind patients of items that are specifically prohibited by NFPA 99 (download poster).
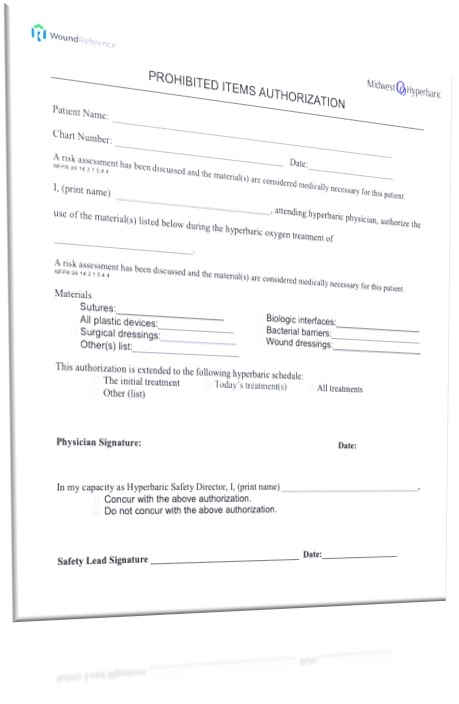
Sample Prohibited Items Authorization Form
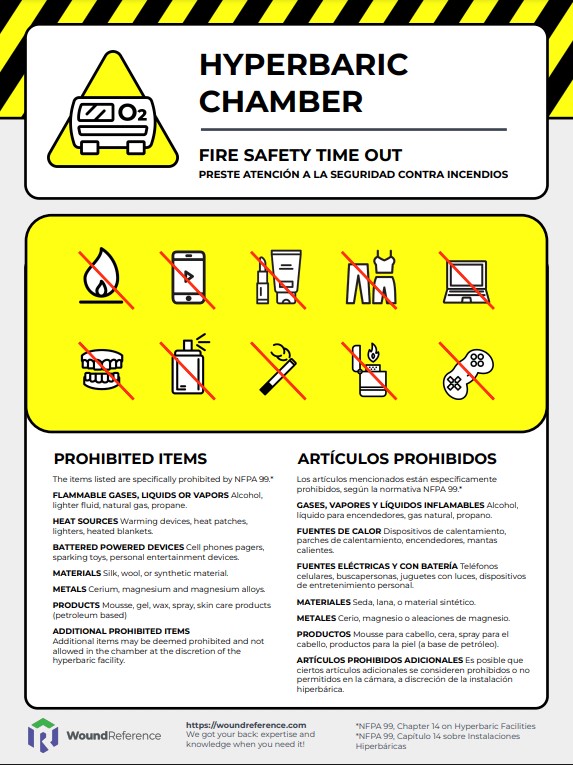 Poster Fire Safety Time Out - Prohibited Items
Poster Fire Safety Time Out - Prohibited Items
OTHER RESOURCES
Official reprint from WoundReference® woundreference.com ©2026 Wound Reference, Inc. All Rights Reserved
NOTE: This is a controlled document. This document is not a substitute for proper training, experience, and exercising of professional judgment. While every effort has been made to ensure the accuracy of the contents, neither the authors nor the Wound Reference, Inc. give any guarantee as to the accuracy of the information contained in them nor accept any liability, with respect to loss, damage, injury or expense arising from any such errors or omissions in the contents of the work.