Summary
A diabetic foot ulcer is a wound or opening in the skin anywhere on the foot (including toes) of a person with diabetes mellitus (that is, with too much sugar in the blood). Diabetic foot ulcers are serious and can lead to more health problems if not cared for properly. Two out of three amputations in the United States happen because of diabetic foot ulcers. Three out of four people who have one of their legs amputated die in 5 years. This is a higher rate of death compared to most cancers.
Treatment and Prevention
Offloading pressure from the diabetic foot ulcer with special footwear, a boot, or a cast is the main form of treatment. To prevent diabetic foot ulcers in people with diabetes, a comprehensive foot evaluation should be done by a primary care physician or podiatrist at least annually (it may be more frequent for people who had diabetic foot ulcers in the past). A prevention plan is recommended by the clinician according to the results of the evaluation.
When to contact your healthcare provider?
Contact your healthcare provider at the first sign of blistering, opening in the skin, or signs of infection.
Patient education handout (download)
|
WHAT is a diabetic foot ulcer?
- Diabetic foot ulcers are serious and can lead to more health problems if not cared for properly. Two out of three amputations in the United States happen because of diabetic foot ulcers. Three out of four people who have one of their legs amputated die in 5 years. This is a higher rate of death compared to most cancers.
- A diabetic foot ulcer is a wound or opening in the skin anywhere on the foot (including toes) of a person with diabetes mellitus (that is, with too much sugar in the blood) (Figure 1).
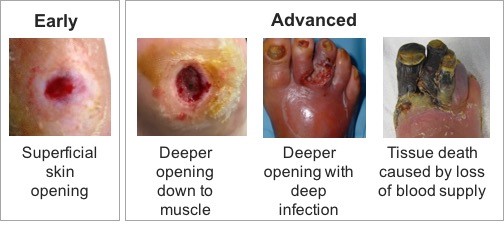
Figure 1. Early and advanced stages of diabetic foot ulcers
WHAT causes a diabetic foot ulcer?
A diabetic foot ulcer can happen because of the changes that diabetes causes in the body. The most important changes in the feet that lead to a diabetic foot ulcer are nerve damage and reduced blood flow. Nerve damage causes changes in skin moisture, foot shape and padding. It also causes the feet to lose protective sensation, that is, the person may not feel pain when stepping on objects, which leads to more feet injuries (Figure 2).
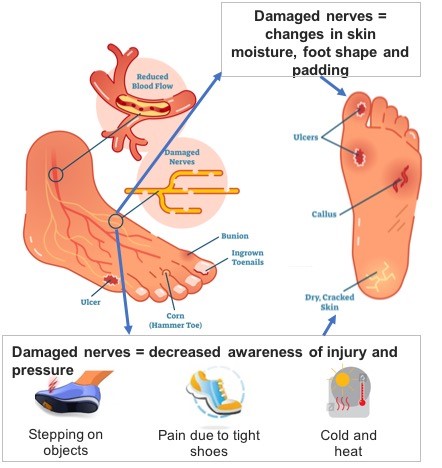 Figure 2. Causes of a diabetic foot ulcer
Figure 2. Causes of a diabetic foot ulcer
HOW do I care for my diabetic foot ulcer?
Diabetic foot ulcers need special care and treatment to prevent infection and to help them heal.
Follow your healthcare provider’s recommendations for wound care which may include:
- Cleaning the wound
- Applying medicine or other treatment to the wound and the surrounding skin
- Covering the wound
- Wearing offloading shoes, boots, or a leg cast that takes pressure off the foot and/or toes
WHAT is "offloading" and why do I need it?
- Offloading is the use of special footwear, a boot, or a cast (offloading device) to relieve pressure from the diabetic foot ulcer during walking.
- If your health care provider suggests that you “offload”, this means you should not walk on the affected limb without a good offloading device.
- Figure 3 illustrates how offloading helps heal diabetic foot ulcers.[1]
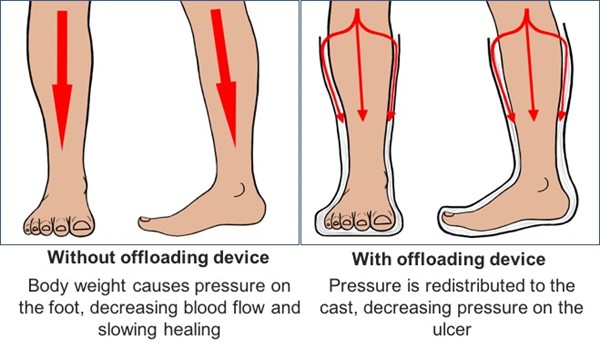
Figure 3. Offloading decreases pressure on foot and helps heal diabetic foot ulcers [1]
WHAT can happen if my diabetic foot ulcer is left untreated?
Patients with diabetes can have decreased blood flow to the feet and toes (poor circulation) due to disease in their arteries which can cause slow healing and increase the risk of infection.
- Infections are a serious complication of diabetic foot ulcers and can lead to bone infections, body infections, and amputation of one or more toes, part of the foot, and/or the leg.
- Amputation is the surgical removal of all or part of a limb or extremity. It is a serious surgical procedure that in some cases may be the best way to control a severe, life-threatening infection.
WHEN should I call my healthcare provider?
Don’t wait or hesitate:
Contact your healthcare provider at the first sign of blistering, opening in the skin, or signs of infection.
Signs of infection include:
- Fevers, chills, nausea, or vomiting
- Unusual increase in blood sugar level
- Increased pain that does not go away
- Redness in and around the wound
- Foot/toes are warm to touch
- Swelling in the leg, foot, or toes
- Increased or unusual wound drainage or odor
HOW can I prevent a diabetic foot ulcer?
Do
- Inspect your feet daily: Look between toes and use a mirror to see the bottom of the feet. Look for red spots, cracks, blisters, calluses, or other changes.
- Inspect your footwear daily: Inspect your shoes for objects such as small pebbles, and inspect socks for holes.
- Protect your feet from injury: Wear properly fitting shoes made for people with diabetes, as well as socks that keep the feet dry.
- Take care of your feet: Wash your feet with soap and water. Dry the feet and between the toes completely after bathing. Apply moisturizer to dry skin as directed, but avoid applying it between the toes
- Care for calluses: Callus removal products and pumice stones may assist with callus management. Speak to your health care provider on the best care for your condition.
- Live a healthy lifestyle and see your primary care physician or podiatrist annually for a foot evaluation: Manage your diabetes by taking medicines as prescribed, eating a well-balanced diet, quitting smoking, and maintaining a healthy weight to reduce your risk of developing a foot ulcer.
Don’t
- Go without protective footwear: Do NOT walk around barefoot or wear socks or thin slippers indoors or outdoors.
- Soak your feet: Soaking your feet can dry out the skin, and hot water may burn your feet without you knowing it.
- Remove or trim ingrown toenails or thick toenails: See a health care provider for management of these conditions.
For more information:
For more information about diabetic foot ulcers, contact your healthcare team. Online resources include:
-
Diabetic Foot Ulcer
-
MedlinePlus.gov