INTRODUCTION
Overview
This topic is part of a document published by the U.S. National Institute for Occupational Safety and Health (NIOSH), which is in the public domain and may be freely copied or reprinted.[1]
All healthcare workers who lift and move patients are at high risk for back injury and other musculoskeletal disorders.[2][3] A work-related musculoskeletal disorder is an injury of the muscles, tendons, ligaments, nerves, joints, cartilage, bones, or blood vessels in the extremities or back that is caused or aggravated by work tasks such as lifting, pushing, and pulling.[4] Symptoms of musculoskeletal disorders include pain, stiffness, swelling, numbness, and tingling.
Home healthcare workers do many of the same tasks as workers in traditional healthcare settings, but conditions in the home setting often make the work more difficult. For instance, home healthcare workers most often perform heavy work, like lifting and moving patients, without assistance.[5]
The following sections define the scope of the problem, discuss risk factors for developing musculoskeletal disorders in home healthcare work, and suggest ways to prevent musculoskeletal disorders.
Background
Relevance
What is the impact of musculoskeletal disorders on the home healthcare industry?
Work-related musculoskeletal disorders are a serious problem in the home healthcare industry.[6] Sprains and strains were the most common lost-work-time injuries to home healthcare workers in 2007.[7] Home healthcare workers may injure themselves when transferring patients into and out of bed or when assisting patients walking or standing.[8] The rate of injury from lifting in 2007 for home healthcare workers was 20.5 per 10,000 workers.[9] Compared with other workers, home healthcare workers take more frequent sick leave as a result of work-related musculoskeletal symptoms.[10][11][12]
Risk factors
Healthcare workers can develop musculoskeletal disorders from any number of common work activities,[13] including the following:
- Forceful exertions (activities that require a person to apply high levels of force, such as during lifting, pushing, or pulling heavy loads)
- Awkward postures when lifting
- Repeated activities without adequate recovery time
Patient-handling tasks often involve motions that challenge a home healthcare worker’s body including twisting, bending, stretching, reaching, and other awkward postures. The most frequent causes of back pain and other injuries among nursing staff (in home healthcare and in hospitals) are lifting and moving patients (“patient transfers”) and bathing, dressing, and feeding patients
[4][14][2]. Healthcare workers who spend the most time transferring, bathing, and dressing patients have the highest rates of musculoskeletal injuries [11][15][16]. In a NIOSH survey study of home healthcare workers, these tasks were identified as significant predictors of pain in the back, neck, shoulders, legs and feet, after adjusting for other factors such as the workers’ age, weight, and physical activities outside of work.[3] It has been
found that frequent heavy lifting, lifting in awkward postures, and lifting without assistance were significant predictors of permanent work disability in home healthcare workers.
What are some factors that complicate patient transfers?
- Incapacity is common among home healthcare patients; about 40% of them have one or more functional limitations because patients are being released after shorter hospital stays and require more intensive care during recovery at home.[17]
- Healthcare workers are commonly required to lift and move patients weighing 90 to 250 pounds. These weights exceed the NIOSH safe lifting limits for both men and women.[18]
- The body weight of a patient is not evenly distributed, nor does a body have convenient hand-holds.
- The patient may be connected to a catheter, I.V., or other equipment, resulting in awkward postures for workers involved in his or her transfer.
- The functional limitations of the patient— physical, mental, or both—may interfere with the lift:
- The patient
may not be able to hold himself or herself up.
- The
patient may not be cooperative.
- The patient may be obese (body mass index
>
30).[19]
- Certain lifting techniques used to minimize the load on the back may increase the load on other body parts such as the neck, shoulders, and arms.[20]
What factors contribute to awkward postures?
- Rooms in patients’ homes are often small or crowded, and workers must often use awkward postures during patient care and transfer tasks.[5] Between 40 and 48% of the home healthcare workers’ time may be spent in poor posture combinations, including forward-bent and twisted postures that are associated with shoulder, neck, and back complaints.[21][22][23] Shoulder and neck symptoms in home healthcare workers have been shown to be due to poor postures and forceful exertions during patient care tasks.[24][25][26][22][20][10][27]
- Beds may not be adjustable, preventing the worker from raising or lowering the patient to the best position for a proper lift.[28] found that problems with the bed’s height, width, placement, and non-adjustability were frequently cited by home healthcare workers as major sources of back stress.
What other factors contribute to musculoskeletal disorders?
- Patients’ homes usually do not have equipment to help with transfers.
- Home healthcare workers frequently endure long periods of standing or walking.
PREVENTION
Can anything help limit musculoskeletal disorders?
The science of work design is called ergonomics. Ergonomics is the design of the work setting (including furniture, tools, equipment, and tasks) to help position the worker in a way that will lesson the possibility of injury when performing work tasks. Therefore, the ergonomics approach optimizes the worker’s safety, health, and performance.
Researchers have found that help from a second trained person reduces the risk of injury during patient-handling tasks but not enough to make the tasks acceptably safe.[29] manual patient handling is “an extremely hazardous job that had substantial risk of causing a low-back injury whether with one or two patient handlers.” For this reason, ergonomic intervention, including the use of electronic and mechanical devices to help with patient transfers, is the most promising approach for reducing low-back injuries during patient handling.
Comprehensive ergonomic interventions using appropriate equipment and training have resulted in dramatic reductions in the incidence and severity of musculoskeletal injuries among healthcare workers. For example, in one study [14], a “zero-lift” program was implemented in seven nursing homes and one hospital to eliminate manual patient transfers: Hoists and other equipment were used to lift patients rather than lifting manually. Injuries related to patient transfers were reduced 39%–79%. Other reductions were noted in the average number of lost workdays (86%), restricted workdays (64%), and workers’ compensation costs (84%). In a review of patient-handling intervention research,[30] identified 21 studies, conducted from 1982 through 2001, that evaluated patient-handling equipment and equipment training. Of the 21 studies, 16 (76%) reported positive effects including reductions in injuries, lost workdays, spinal loads, harmful postures, perceived exertion, and staffing requirements. Subsequent studies have cited similar positive effects for healthcare workers as well as positive effects on the quality of patient care.[31][32][33][34][35][36][37][38][39] Nelson et al. summarize numerous other case studies using ergonomic interventions in hospitals and nursing homes that have also shown large reductions in injury rates, workers’ compensation costs, medical costs, insurance premiums, and lost and restricted workdays.[19]
Whenever possible, devices should be used to help with patient transfers. Various devices such as draw sheets, slide boards, rollers, slings, belts, and mechanical or electronic hoists (to lift the patient) have been designed to assist healthcare workers and patients. The main lesson to be learned from studies about such devices is that each home situation must be assessed separately to find out which device will be the most suitable for (1) the persons using it, (2) the place(s) it will be used, and (3) the task(s) for which it will be used.[40][15][41] Recognizing the importance of ergonomics for protecting the safety of healthcare workers, the Occupational Safety and Health Administration (OSHA) has issued ergonomics guidelines for nursing homes that emphasize the proper use of assistive devices during patient handling.[42] In addition, the VISN 8 Patient Safety Center of Inquiry[43] has published a resource guide about safe patient handling and movement. The guide describes assistive devices and elements of an ergonomics program that have been tested within the Veterans’ Health Administration and are being used on an ongoing basis at many other inpatient healthcare facilities. Some of the information from these sources is specific to nursing homes and hospitals, yet much of it applies to home healthcare. Parsons [44][45] has written two articles specifically about preventing musculoskeletal disorders in home healthcare workers.
Figures 1 through 10 provide examples of assistive devices that can be used in home settings. Many more types of products designed for a variety of patient-handling and other home healthcare needs are commercially available. Patients, family members, and home healthcare workers should consult with equipment vendors and the patient’s primary doctor to select proper assistive devices that will lessen the worker’s strain without decreasing the patient’s safety or comfort. In some cases, a prescription is required to get such devices. Generally, a patient’s insurance at least partially covers the costs. It’s most important that all persons who use a lifting device be fully trained to use it safely. Periodic maintenance and cleaning for some devices, such as hoists, are required.
What can I do to prevent musculoskeletal disorders?
Some simple solutions have greatly reduced the number of patient transfers that nursing personnel need to perform. For example, a study found that using a hoist with a built-in weighing scale eliminated transfers for the sole purpose of weighing the patient (from wheelchair to weighing scale and from weighing scale to wheelchair) and using a rolling toileting or showering chair reduced the six transfers needed for toileting and showering (bed to wheelchair, wheelchair to toilet, toilet to wheelchair, wheelchair to bathtub, bathtub to wheelchair, and wheelchair to bed) to two transfers (bed to toileting/showering chair and toileting/showering chair to bed).[40]
Equipment such as adjustable beds, raised toilet seats, shower chairs, and grab bars are also helpful for reducing musculoskeletal risk factors. This type of equipment keeps the patient at an acceptable lift height and allows the patient to help himself or herself during transfer when possible.
Even when assistive devices are used during patient care, it is impossible to completely eliminate the need for some amount of physical exertion. For example, when using a hoist, the healthcare worker must move the patient in order to fasten the sling, and workers must support and balance the patient while using hoists and other devices. These tasks will always pose some risk of injury.[43] To lessen the risk, certain principles of body mechanics should be followed as much as possible to avoid harmful postures.[46][47][40][16][19] Some strategies for effective body mechanics in patient handling are described in the Recommendations for Workers.

Figure 1 . Slide/transfer board (Copyright by Sammons Preston Rolyan. Reprinted with permission.)

Figure 2. Slide/draw sheet (Copyright by SureHands Lift and Care Systems. Reprinted with permission.)

Figure 3 . Patient moving sling (Copyright by Sammons Preston Rolyan. Reprinted with permission.)

Figure 4 . Rolling toilet/shower chair (Copyright by Sammons Preston Rolyan. Reprinted with permission.)

Figure 5 . Gait/walking belt (Copyright by Sammons Preston Rolyan. Reprinted with permission.)

Figure 6 . Stationary shower chair (Copyright by Sammons Preston Rolyan. Reprinted with permission.)

Figure 7 . Raised toilet seat (Copyright by Sammons Preston Rolyan. Reprinted with permission.)

Figure 8 . Grab bars (Copyright by Sammons Preston Rolyan. Reprinted with permission.)

Figure 9 . Rotation disk (Copyright by Sure Hands Lift and Care Systems. Reprinted with permission.)
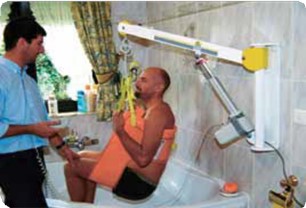
Figure 10 . Wall sling (Copyright by Sure Hands Lift and Care Systems. Reprinted with permission.)
Recommendations for Employers
- Consult with a professional with expertise in patient-care ergonomics to determine when assistive devices are necessary and to provide training on proper use of the equipment.
- Provide ergonomic training for workers.
- Evaluate each patient-care plan to determine whether ergonomic assistive devices are appropriate.
- Provide ergonomic assistive devices when needed.
- Reassess the training, the care plan, and the assistive devices once installed and in use by the caregiver.
Bringing ergonomic approaches into home healthcare settings is challenging because of the following:
- Workers may think assistive devices will be difficult to work with and time-consuming.
- Patients and family caregivers may fear that assistive devices will be unsafe or uncomfortable.
- Patients and families may be unwilling or unable to accept changes in the home.
- A device may be too expensive for the patient and family.
If patients and families are resistant to installing or buying an assistive device, the employers should inform them about the risks involved in moving patients when a device is not used. These risks may include the following:
- An overexerted worker could accidentally harm the patient.
- The patient may be injured by being dropped, jared, or not properly handled during unassisted transfers.
Recommendations for Workers
Workers can follow these recommendations [46][47][16][19]:
- Use ergonomic assistive devices if they are available.
- Move along the side of the patient’s bed to stay in safe postures while performing tasks at the bedside. Do not stand in one location while bending, twisting, and reaching to perform tasks.
- When you are manually moving the patient, stand as close as possible to the patient without twisting your back, keeping your knees bent and feet apart. To avoid rotating the spine, make sure one foot is in the direction of the move.
- Use a friction-reducing device such as a slip sheet whenever possible.[19] Using gentle rocking motions can also reduce exertion while moving a patient.
- Pulling a patient up in bed is easier when the head of the bed is flat or down. Raising the patient’s knees and encouraging the patient to push (if possible) can also help.
- Apply anti-embolism stockings by pushing them on while standing at the foot of the bed. This position reduces exertion compared with standing at the side of the bed.
Notify your employer if you feel you would benefit from additional training or ergonomic assistive devices.
RESOURCES
- CDC. Preventing falls among seniors (topic page) [www.cdc.gov/ncipc/duip/spotlite/fallpub.htm].
- NIOSH [2006]. Safe lifting and movement of nursing home residents. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2006–117 [www.cdc.gov./niosh/docs/2006–117/].
- OSHA. Healthcare wide hazards module— ergonomics [www.osha.gov/SLTC/etools/ hospital/hazards/ergo/ergo.html].
Official reprint from WoundReference® woundreference.com ©2026 Wound Reference, Inc. All Rights Reserved
NOTE: This is a controlled document. This document is not a substitute for proper training, experience, and exercising of professional judgment. While every effort has been made to ensure the accuracy of the contents, neither the authors nor the Wound Reference, Inc. give any guarantee as to the accuracy of the information contained in them nor accept any liability, with respect to loss, damage, injury or expense arising from any such errors or omissions in the contents of the work.