SUMMARY
Arterial or ischemic ulcers, are a wound or opening in the skin due to poor blood circulation because of narrowed or damaged arteries (arterial insufficiency). The ulcers commonly occur along the legs, feet, or toes.
This topic explains what causes arterial ulcers, and how they can be managed and prevented.
When to contact your healthcare provider?
Contact your provider if:
- Your foot/leg becomes painful, seems white or purple, has decreased pulses, feels cold, feels numb or hard to move
- Your foot/leg shows redness, blistering, a new opening in the skin, or signs of infection
- You have 3 days’ or less worth of dressing supplies.
WHAT is an arterial ulcer?
Arterial or ischemic ulcers, are a wound or opening in the skin due to poor blood circulation because of narrowed or damaged arteries (arterial insufficiency). The ulcers commonly occur along the legs, feet, or toes.
WHAT causes an arterial ulcer?
Peripheral artery disease (PAD) causes most arterial ulcers. PAD commonly occurs in patients with diabetes mellitus, high blood pressure, heart disease, high cholesterol, smokers, and in several other medical conditions. See Figures 1 and 2.
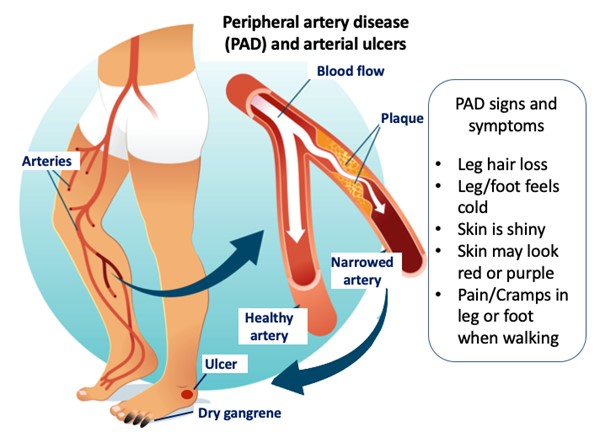
Fig. 1. Peripheral artery disease and arterial ulcers
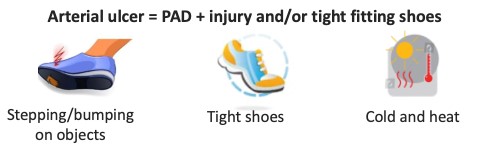
Fig. 2. Arterial ulcers precipitating factors. Arterial ulcers may occur on an injured leg/foot with poor blood perfusion
HOW is the condition treated?
Improving the supply of blood is the primary treatment for arterial ulcers. Methods to improve circulation include:
- Angioplasty: a balloon is inserted and inflated in the narrow artery and pushes the plaque against the artery wall. The artery widens and allows for greater blood flow.
- Endarterectomy: Artery plaque is surgically removed from the narrow artery.
- Arterial Bypass: A healthy piece of artery is removed (graft) and reconnected to “reroute” the supply of blood away from the diseased artery.
- Hyperbaric Oxygen Therapy: While in an enclosed vessel, patients breath in oxygen at a pressure greater than sea level resulting in increased oxygen in the blood and tissues.
- Medications: Medication may be prescribed that reduces blood platelets, cholesterol, high blood pressure, and high blood sugars.
- Smoking cessation: Quitting smoking improves oxygen in the blood.
- Exercise: If tolerated and allowed by your provider
HOW do I care for my arterial ulcer?
Arterial ulcers need special care and treatment to prevent infection and to help them heal.
Follow your healthcare provider’s recommendations for wound care which may include:
- Applying medicine or other treatment to the wound and the surrounding skin
- Wearing protective footwear that take pressure off the foot and/or toes
HOW can I alleviate pain?
Speak to your healthcare provider regarding pain management relief. Depending on the type of pain and its frequency, oral and topical medications are available.
WHAT can happen if my arterial ulcer is left untreated?
- Patients with arterial ulcers can have slow healing and are at increased risk of infection since the specialized cells in the blood that heal wounds and treat infections have difficulty reaching the wound.
- Infections are a serious complication of arterial wounds and can lead to bone infections, body infections, and amputation of the toes, part of the foot, and/or the leg.
- Amputation is the surgical removal of all or part of a limb or extremity. It is a serious surgical procedure that in some cases may be the best way to control a severe, life-threatening infection.
WHEN should I contact my healthcare provider?
Don’t wait or hesitate to contact if:
- Your foot/leg becomes painful, seems white or purple, has decreased pulses, feels cold, feels numb or hard to move
- Your foot/leg shows redness, blistering, a new opening in the skin, or signs of infection
- You have 3 days’ or less worth of dressing supplies.
Signs of infection include:
- Fevers, chills, nausea, or vomiting
- Unusual increase in blood sugar level
- Increased pain that does not go away
- Redness in and around the wound
- Leg/foot/toes are warm to touch
- Swelling in the leg, foot, or toes
- Increased or unusual wound drainage or odor
HOW can I prevent an arterial ulcer?
Do
- Inspect your legs and feet daily: Look at all aspects of the legs, feet, and between toes. Use a mirror to see the bottom of the feet and the back of the legs. Look for red spots, cracks, blisters, calluses, or other changes.
- Inspect your footwear daily: Inspect your shoes for objects such as small pebbles, and inspect socks for holes.
- Protect your legs and feet from injury: Wear properly fitting clothing and shoes. Wear diabetic shoes if you have diabetes, as well as socks that keep the feet dry.
- Take care of your legs and feet: Wash your legs and feet with soap and water. Dry the legs, feet, and between the toes completely after bathing. Apply moisturizer to dry skin as directed, but avoid applying it between the toes.
- Live a healthy lifestyle and see your primary care physician or podiatrist for yearly foot evaluation: Manage your diabetes by taking medicines as prescribed, eat a well-balanced diet, quit smoking, and maintain a healthy weight to reduce your risk of developing arterial ulcers.
Don’t
- Go without protective leg or footwear: Do NOT walk around barefoot or wear thin slippers indoors or outdoors. Wear protective clothing to avoid injury to the legs.
- Soak your feet: Soaking your feet can dry out the skin, and hot water may burn your feet or legs without you knowing it.
- Remove or trim ingrown toenails or thick toenails: See a health care provider for management of these conditions.